Symptomatic Unilateral Lumbosacral Transitional Vertebrae: Clinical and Imaging Assessment..
Rajan R Murgai , Skorn Ponrartana , Lindsay M Andras and David L Skaggs
DOI10.36648/2471-8173.21.7.25
Rajan R Murgai1, Skorn Ponrartana2, Lindsay M Andras1 and David L Skaggs3*
1Children’s Orthopaedic Center, Children’s Hospital, Los Angeles, CA, USA
2Department of Radiology, Children’s Hospital, Los Angeles, CA, USA
3Cedars-Sinai Spine Center, Los Angeles, CA, USA
- Corresponding Author:
- David L. Skaggs
Cedars-Sinai Spine Center
Los Angeles, CA, USA
Tel: 3104236665
Fax: 4243146414
E-mail: david.skaggs@cshs.org
Received Date: June 21, 2021; Accepted Date: July 16, 2021; Published Date: July 26, 2021
Citation: Murgai RR, Ponrartana S, Andras LM, Skaggs DL (2021) Symptomatic Unilateral Lumbosacral Transitional Vertebrae: Clinical and Imaging Assessment. Spine Res. Vol.7 No.7:25
Abstract
Introduction: LSTV are common spinal anomalies whose clinical significance and association with low back pain (LBP) are controversial. Differentiating LSTV from other sources of LBP is essential in guiding treatment. The purpose of this study was to identify clinical and imaging features associated with symptomatic unilateral LSTV in a pediatric patient population.
Methods: A retrospective review of patients with LBP and presumed symptomatic unilateral LSTV at a tertiary pediatric hospital from 2014 – 2017 was conducted. Patients 18 years or younger were included. LSTV were considered symptomatic if there was localized pain during activities of daily living and localized ipsilateral pain in extension at the LSTV.
Results: 6 patients with LBP and symptomatic unilateral LSTV were identified. Edema at the pseudoarthrosis was only noted on a fluid sensitive sequence with fat suppression (STIR) MRI of the lumbar spine. 3/3 patients with STIR had evidence of edema at the pseudoarthrosis. 2/2 patients with bone scintigraphy with SPECT imaging had increased radiotracer activity at the pseudoarthrosis.
Discussion: Symptomatic unilateral lumbosacral transitional vertebrae (LSTV) may present with localized ipsilateral pain exacerbated by lumbar extension. Coronal STIR sequence MRI of the lumbar spine most effectively demonstrated edema at the pseudoarthrosis, though it could also be noted in sagittal STIR sequences. Increased radiotracer uptake at the pseudoarthrosis on bone scintigraphy with SPECT imaging was also observed.
https://maviyolculuk.online/
https://mavitur.online/
https://marmaristeknekirala.com.tr
https://tekneturumarmaris.com.tr
https://bodrumteknekirala.com.tr
https://gocekteknekirala.com.tr
https://fethiyeteknekirala.com.tr
Level of Evidence: IV
Keywords
Transitional vertebra; Low back pain; Bertolotti's syndrome; STIR Magnetic resonance imaging; Transitional lumbosacral segment
Introduction
Low back pain is common in adolescents and can be debilitating. The reported prevalence of low back pain in adolescents 9-16 years of age ranges from 11.6% to 85.6% [1]. It can have a significant impact on this patient population through restriction of activities of daily living and is a risk factor for developing low back pain as an adult [2,3]. The etiology of low back pain in these patients is often undetermined. A prospective study of 73 pediatric patients with a minimum of 3 months of low back pain found that 78.1% of patients lacked a definitive diagnosis after two years [4]. This study examines one potential source of low back pain in this patient population, lumbosacral transitional vertebrae (LSTV).
LSTV are congenital anomalies in which the transverse process of the lowest lumbar vertebra has partial or total fusion with the sacrum [5]. Transitional vertebrae are estimated to exist in 7% to 36% of the population, with unilateral anomalies being the most common [6-11]. Several studies have established an association between LSTV and low back pain [7,9]. However, others have questioned this relationship [8,12,13]. The association of low back pain with LSTV, Bertolotti’s syndrome, remains controversial.
Due to the wide prevalence of LSTV and low back pain, physicians must be able to differentiate symptomatic LSTV from other possible sources of low back pain [14]. Correct determination of the etiology of low back pain in patients with LSTV is essential for guiding treatment [15]. While the clinical assessment and imaging features of patients with symptomatic LSTV have been studied in adults, few studies have focused on LSTV in the pediatric patient population [16-18]. The purpose of this study was to identify clinical characteristics and imaging features of symptomatic unilateral L5-S1 transitional vertebrae in pediatric patients.
Materials and Methods
A retrospective review of patients who presented with low back pain and were found to have LSTV at a tertiary pediatric hospital from 2014 to 2017 was conducted. LSTV were considered symptomatic if there was localized pain during activities of daily living and localized ipsilateral pain in extension at the LSTV. Patients 18 years or younger were included. Patients were identified by the senior author. Institutional Review Board approval was obtained for this study. Each patient’s medical chart was reviewed for characteristics of pain (duration, localization, activity limitation, progression, radiation, episodes of sciatica) and physical exam findings (pain with lumbar extension, straight leg test, neurologic exam). Patient demographic information such as sex and age were also collected.
Imaging analysis
Anteroposterior and lateral radiographs of the lumbar spine were performed using standard technique. All but one subject had a limited focused CT scan from L4-S2 that was obtained helically with 0.625 mm slices and reformatted at 2.5 mm in the axial plane, 1 mm in the coronal plane, and 1 mm in the sagittal plane. Additionally, axial reformats of each vertebral body with the plane parallel through the vertebral body was performed at 1 mm slices. Three-dimensional reconstruction of the lumbar spine was also performed. MRI studies were performed at different institutions with varying protocols. The MRI sequences of the lumbar spine performed are listed in Table 1.
| Case No. | Sagittal T TSEa 1 |
Sagittal T TSEb 2 |
Axial T2 TSEc |
Coronal T TSEd 2 |
Sagittal STIRe | Coronal STIRf |
|---|---|---|---|---|---|---|
| 1 | x | x | x | x | x | |
| 2 | x | x | x | x | x | x |
| 3 | x | x | x | x | ||
| 4 | x | x | x | x | ||
| 5 | x | x | x | x | ||
| 6 | x | x | x | x | x | x |
=90-120, slice thickness= 4.5-5 mm, interval=0-1 mm, field of view=300- 400, matrix=256-392/209-343, number of excitations= 1-2; e: TR=2500- 3800, TE =54-70, slice thickness= 4 mm, interval=0.4-1 mm, field of view=270-340, matrix=256-400/192-317, number of excitations= 1; f: TR=3806, TE =80, slice thickness= 3 mm, interval=0 mm, field of view=200, matrix=256/222, number of excitations= 1-1.5
Table 1 MRI sequences of the lumbar spine performed.
In two subjects, Technetium -99m bone scintigraphy was performed. After 2-4 hours of intravenous administration of technetium-99m MDP (14.2 mCi and 16.3 mCi) a whole-body planar scintigraphy image was acquired. Routine single-photon emission computed tomography (SPECT) images of the abdomen and pelvis were also obtained. A pediatric neuroradiologist with 5 or more years of experience evaluated all images.
Results
Six patients with low back pain and presumed symptomatic unilateral LSTV were identified. Mean patient age was 14.5 (range, 13 to 16 years old). There were 5 female patients and 1 male patient.
Clinical assessment
All patients localized their pain to their low back ipsilateral to the LSTV. 67% (4/6) of patients reported activity limitations and 50% (3/6) of patients reported progressive pain. The duration of patient’s symptoms ranged from 5 days to 24 months with a mean of 10.7 ± 9.1 months. Two patients had minor trauma at onset of low back pain. One patient had episodes of sciatica, pain that radiated to their leg on the same side as their LSTV, and a positive straight leg raise. On physical exam, all patients had localized ipsilateral pain with lumbar extension at the LSTV. All patients had a normal neurologic exam (Table 2).
| Case No. | Sex | Age | Side LSTV | Duration (months) | Pain Localization |
Activity Limitation | Progressive Pain |
Pain with Extension |
Radiating Pain |
Episodes of Sciatica |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 13 | Left | 3 | Left | Yes | Yes | Yes | No | No |
| 2 | F | 14 | Left | 7 | Left | Yes | No | Yes | No | No |
| 3 | F | 14 | Left | 18 | Left | No | No | Yes | No | No |
| 4 | M | 16 | Left | 0.17 | Left | Yes | No | Yes | No | No |
| 5 | F | 14 | Right | 12 | Right | Yes | Yes | Yes | No | No |
| 6 | F | 16 | Left | 24 | Left | No | Yes | Yes | Yes | Yes |
Table 2 Clinical findings of study subjects.
Imaging analysis
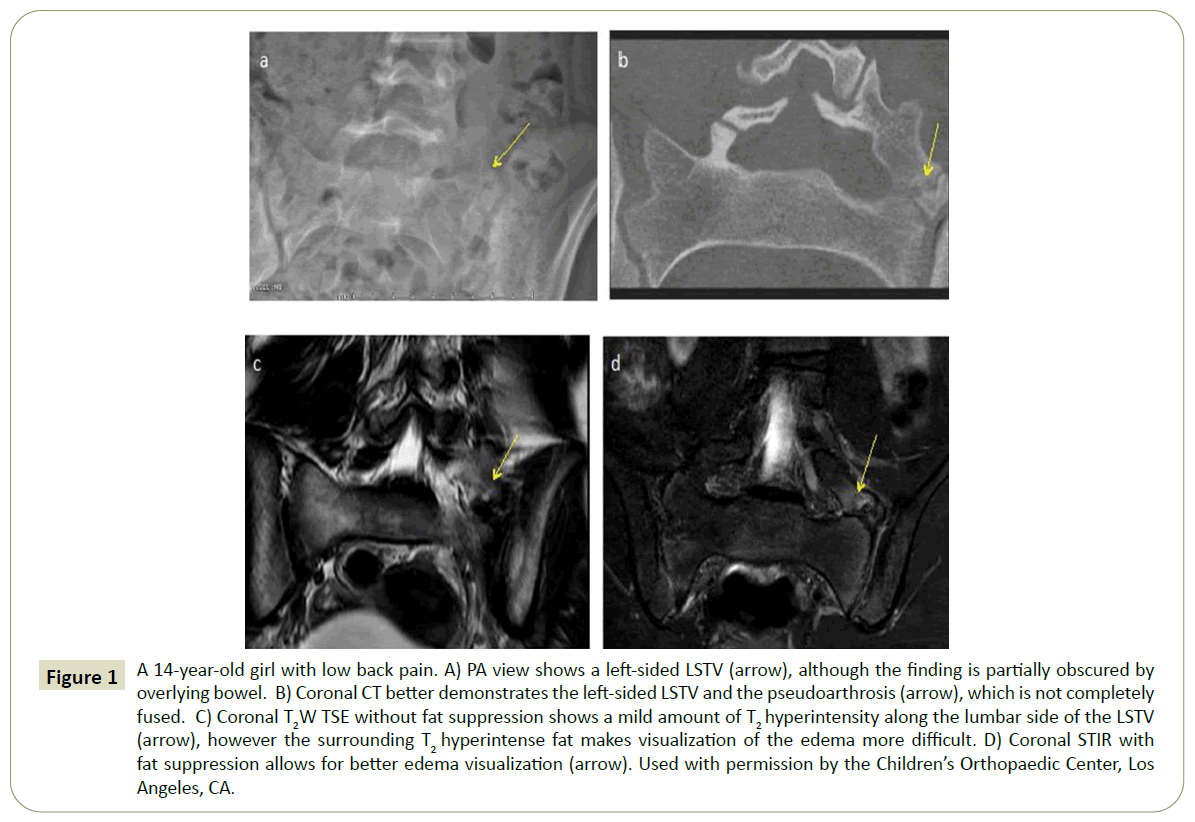
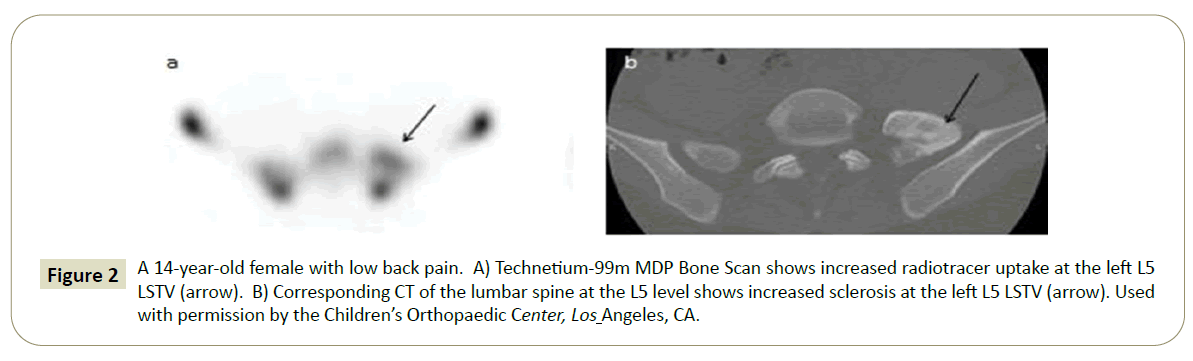
Only 3 of these patients had plain radiographs of the lumbar spine and the LSTV were detected in 67% (2/3) of those cases. Five patients had a limited CT scan. LSTV and sclerosis at the pseudoarthrosis were detected in all cases where CT was performed (6/6) (Table 3). There were also 3 patients who had an MRI of the lumbar spine with an additional STIR (short tau inversion recovery) sequence performed. Of those 3, none of the patients had evidence of bone marrow edema at the pseudoarthrosis on MRI T2 TSE imaging of the lumbar spine. In all 3 cases, the sagittal STIR images demonstrated bone marrow edema at the pseudoarthrosis. Two of these patients had additional coronal STIR images which better demonstrated bone marrow edema at the pseudoarthrosis (Figure 1). Bone scintigraphy with SPECT imaging was performed in two cases and in both cases showed increased radiotracer activity at the pseudoarthrosis (Figure 2).
| Case No. | XR | CT | MRI | MRI w/ STIR | Bone Scintigraphy |
|---|---|---|---|---|---|
| 1 | Not Performed | Left L5 transverse process Sacralization | No edema observed | Edema at the pseudoarthrosis | Increased radiotracer activity at pseudoarthrosis |
| 2 | Not Performed | Left L5 transverse process sacralization | No edema observed | Edema at the pseudoarthrosis | Not performed |
| 3 | Left L5 transverse process sacralization | Left L5 transverse process sacralization | No edema observed | Not performed | Not performed |
| 4 | Left L5 transverse process sacralization | Not Performed | No edema observed | Not performed | Not performed |
| 5 | No LSTV observed | Right L5 transverse process sacralization |
No edema observed | Not performed | Increased radiotracer activity at pseudoarthrosis |
| 6 | Not Performed | Left L5 transverse process sacralization | No edema observed | Edema at the pseudoarthrosis | Not performed |
Table 3 Imaging findings of study subjects.
Figure 1: A 14-year-old girl with low back pain. A) PA view shows a left-sided LSTV (arrow), although the finding is partially obscured by overlying bowel. B) Coronal CT better demonstrates the left-sided LSTV and the pseudoarthrosis (arrow), which is not completely fused. C) Coronal T2W TSE without fat suppression shows a mild amount of T2 hyperintensity along the lumbar side of the LSTV (arrow), however the surrounding T2 hyperintense fat makes visualization of the edema more difficult. D) Coronal STIR with fat suppression allows for better edema visualization (arrow). Used with permission by the Children’s Orthopaedic Center, Los Angeles, CA.
Figure 2: A 14-year-old female with low back pain. A) Technetium-99m MDP Bone Scan shows increased radiotracer uptake at the left L5 LSTV (arrow). B) Corresponding CT of the lumbar spine at the L5 level shows increased sclerosis at the left L5 LSTV (arrow). Used with permission by the Children’s Orthopaedic Center, Los Angeles, CA.
Discussion
Low back pain in adolescents can significantly worsen quality of life [19]. LSTV are common spinal anomalies whose clinical significance and association with low back pain are controversial. Low back pain in the setting of a LSTV should not usually be attributed to the vertebral anomaly given their widespread prevalence. Early diagnosis of an asymptomatic LSTV should not lead to additional work-up or follow-up as the natural history is usually benign. In this study cohort, 67% (4/6) of patients reported activity limitations and 50% (3/6) of patients reported progressive pain. Accurate identification of LSTV and correlation with clinical symptoms is essential to avoid unnecessary procedures [15]. This study identifies clinical and imaging characteristics of symptomatic unilateral LSTV in the pediatric population.
The exact etiology of the low back pain secondary to LSTV is unclear. Several studies suggest that the abnormal biomechanics of transitional vertebrae contribute to the development of low back pain [20-22]. Some authors have suggested that asymmetric biomechanics observed in unilateral transitional vertebrae may lead to degenerative changes in the contralateral facet joint [21]. Transitional vertebrae may also increase stability at the fused transitional level and cause hypermobility above the transitional segment [23]. These abnormal biomechanics may trigger accelerated disc disease (degeneration, annular tears, herniation, etc.) in the first disc cephalad to the LSTV due to increased biomechanical strain. Several studies have shown that LSTV are protective from disc disease at the level of the transitional vertebrae but lead to more disc disease at the level above the LSTV. Furthermore, Castellvi classification correlates with this effect, with Type II LSTV being less protective at the level of transition and less harmful to the cephalad disc [4,7,10-12] (Table 4).
| Castellvi type | Definition |
|---|---|
| Type I | Dysplastic transverse process |
| Type II | Enlarged transverse process with pseudoarthrosis with the adjacent sacral ala |
| Type III | Enlarged transverse process with complete fusion with the adjacent sacral ala |
| Type IV | Type II on one side, Type III on the other |
Table 4 Castellvi classification of LSTV [5].
Another possibility is that the low back pain may be due to degenerative changes at the pseudoarthrosis. Nardo et al. found that patients with Castellvi Type II and IV LSTV had a higher prevalence of low back pain and buttock pain than those without transitional vertebrae [9]. This is thought to be due to the pseudoarticulation of the transverse process to the sacrum that occurs in Castellvi Type II and IV LSTV. Tang et al. reported similar results in a study of 5,860 individuals [7]. Additionally, one of the patients in this series reported unilateral radicular symptoms on the same side of their LSTV and had a positive straight leg test. Transitional vertebrae have also been associated with lumbosacral nerve root symptoms due to spinal canal stenosis or extraforaminal stenosis [24,25].
Few studies have examined the clinical characteristics associated with symptomatic LSTV. Two studies found that patients with LSTV were more likely to report buttock pain than patients without LSTV [7,9]. Nardo et al. found that patients with type 2 and 4 LSTV were more likely to report middle or upper back pain, higher pain frequency and severity, and lower physical activity levels than patients without LSTV [9]. Conversely, Murtaugh et al. found no difference in the proportion of leg pain, foot pain, positive straight leg test, and neurologic findings between patients with and without LSTV [26]. To our knowledge, no studies to date have reported localized ipsilateral low back pain exacerbated by lumbar extension as a clinical sign of symptomatic LSTV.
Transitional vertebrae can be identified on PA radiographs, CT, or MRI. However, transitional vertebrae are often inaccurately identified and categorized with MRI and standard PA radiographs [27,28]. In this study, there was one patient that was detected to have a LSTV on CT that was not detected on plain PA radiographs. CT appears to be the optimal imaging technique for the classification of LSTV due to its excellent spatial resolution [15]. CT imaging revealed sclerosis at the pseudoarthrosis in 5 of these patients and also allowed for evaluation of sclerotic changes in close proximity to the pseudoarthrosis, implying slight motion and degenerative changes. Other authors have also suggested that CT is the most sensitive test for diagnosis of LSTV, however without a large number of patients with a full complement of multiple imaging studies we are not able to truly assess the sensitivity of CT scan compared to other imaging modalities [14].
In the patients diagnosed with LSTV who had an MRI of the lumbar spine with a STIR sequence bone marrow edema was present (3/3). In a study of patients with chronic back pain and suspected axial spondyloarthritis, de Bruin et al. found bone marrow edema on MRI with a STIR sequence in 13% of patients with LSTV and no patients without LSTV [29]. LSTV were not found to be associated with axial spondyloarthritis. The bone marrow edema was localized to the immediate articulating surfaces of the LSTV unlike the bone marrow edema of the sacroiliac joints typically associated with axial spondyloarthritis. Additionally, the patients with type II or IV LSTV had the highest prevalence of bone marrow edema suggesting that pseudoarticulation was more likely to cause reactive changes than complete fusion [29]. In a study of patients with low back pain, Friedrich et al. found a strong correlation between a patient’s change in pain score and intensity of edema visualized at the facet joints on MRI STIR sequences [30]. However, it remains unclear as to whether the presence of bone marrow edema correlates with low back pain.
In both patients whom SPECT imaging was performed, increased radiotracer uptake was observed at the pseudoarthrosis. In a study of 6 to 19 year-old patients with LSTV and low back pain, Connolly et al. found increased radiotracer uptake at the transverse-sacral articulation on SPECT imaging in 81% of patients [17]. Similarly, Pekindil et al. performed SPECT imaging on patients with LSTV and found focal markedly increased uptake in patients with back pain and degenerative changes. However, they found only mildly increased uptake in patients with degenerative changes who lacked low back pain [31]. Thus, focal markedly increased radiotracer uptake on SPECT imaging may help identify degenerative changes associated with pain secondary to LSTV.
Ideally Bone Scintigraphy should not need to be performed as it has radiation, and a coronal stir image of an MRI should be able to identify increased metabolic activity at the site of a symptomatic transitional vertebrae. Plain x-rays are usually the first imaging study, but can miss many causes of back pain, as well as not give definitive evidence of a LSTV. An MRI should be able to define both boney and cartilaginous LSTV without radiation so it is likely the most important study, and if a LSTV is suspected a coronal stir sequence should be obtained. A CT scan is useful particularly in cases of backpain with extension as a CT scan is the gold standard to identify other causes of back pain such as facet fractures and spondylolysis which could both be missed on MRI.
Previous studies have found an injection of steroids or local anesthetic into the pseudoarthrosis site to have diagnostic and therapeutic value. In a series of 10 patients with LBP and LSTV, Marks et al. found that steroid and anesthetic injections into the pseudoarthrosis provided immediate pain relief in 9 patients, with one patient remaining pain free at two years [32]. In a study of patients with LSTV and LBP temporarily relieved by diagnostic injections into the pseudoarthrosis, Li et al. found that resection of the LSTV provided pain relief [33]. The author did not consider patients who failed to respond to these injections to be surgical candidates. Diagnostic injections were not attempted with any of the patients in our series.
Limitations to this study include the small sample size of patients and lack of control group making it difficult to draw definitive conclusions. However, this study identifies clinical and imaging features of an underreported source of low back pain in pediatric patients and provides the framework for future studies to enhance its diagnosis. This study identified localized ipsilateral low back pain that is exacerbated by lumbar extension as clinical features suggestive of symptomatic LSTV. In patients whom symptomatic LSTV are suspected that are undergoing an MRI, we recommend examining a coronal STIR sequence, as edema at the pseudoarthrosis was most evident on this sequence. Future studies are needed to assess whether the presence of bone marrow edema at the pseudoarthrosis correlates with low back pain or is a predictor of which patients would benefit from surgical intervention.
While previous studies suggest that CT is the most sensitive imaging technique for the characterization of LSTV, we are not able to compare the sensitivity of CT to other imaging modalities without a large number of patients with a full complement of studies [14,15]. Due to radiation concerns, we do not recommend routine CT scans. However, obtaining a CT scan in the very rare potential surgical cases may be beneficial [15].
Increased radiotracer uptake at the site of pseudoarthrosis on SPECT imaging is suggestive of this condition, however, whether this increased uptake on SPECT imaging provides additional prognostic information remains to be determined. As SPECT imaging has radiation, with unclear benefit over observing inflammation or degenerative changes on an MRI, we do not recommend routine SPECT imaging.
The purpose of this study is to describe the presentation, physical exam and imaging findings of symptomatic LSTV. We encourage clinicians treating adolescent patients with low back pain to consider LSTV as a potential etiology and to be cognizant of this when reviewing CT, MRI, or bone scans obtained for evaluation of these patients, especially in the setting of back pain with extension.
Conflict of Interests
Author D
Research Grants: Pediatric Orthopaedic Society of North America & Scoliosis Research Society, Paid to Columbia University; Ellipse (Co-PI, Paid to Growing Spine Foundation); Consulting: Zimmer, Biomet; Grand Rounds (a healthcare navigation company); Stocks options: Zipline Medical, Inc.; Green Sun Medical; Stocks: Orthobullets; Board Membership: Growing Spine Study Group, Growing Spine Foundation; Paid Lecturer: Zimmer, Biomet; Patents: with Medtronic & ZimmerBiomet; Royalties: Wolters Kluwer Health - Lippincott Williams & Wilkins; Biomet Spine; Editor: Orthobullets, Co-Editor in Chief; Editorial boards: Spine Deformity, Orthopedics Today, Journal of Children’s Orthopedics
Author C
Biomet: Paid consultant; Paid presenter or speaker; Eli Lilly: Stock or stock Options; Journal of Pediatric Orthopedics: Editorial or governing board; Medtronic: Paid consultant; Paid presenter or speaker; Nuvasive: Paid consultant; Paid presenter or speaker; Orthobullets: Publishing royalties, financial or material support; Pediatric Orthopaedic Society of North America: Board or committee member; Scoliosis Research Society: Board or committee member; Zimmer: Paid consultant
Authors A and B declare they have no conflict of interest.
This study has been carried out with approval from the Committee on Clinical Investigations at Children’s Hospital Los Angeles, CA, USA.
References
- Calvo-Muñoz I, Kovacs FM, Roqué M, Gago Fernandez I, Seco Calvo J (2018) Risk Factors for Low Back Pain in Childhood and Adolescence. Clin J pain 34: 468-484.
- Hestbaek L, Leboeuf-Yde C, Kyvik KO, Manniche C (2006) The course of low back pain from adolescence to adulthood: eight-year follow- up of 9600 twins. Spine 31: 468-472.
- Fritz JM, Clifford SN (2010) Low back pain in adolescents: a comparison of clinical outcomes in sports participants and nonparticipants. J Athl Train 45: 61-66.
- Bhatia NN, Chow G, Timon SJ, Watts HG (2008) Diagnostic modalities for the evaluation of pediatric back pain: a prospective study. J Pediatr Orthop 28: 230-233.
- Castellvi AE, Goldstein LA, Chan DP (1984) Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine 9: 493-495.
- Paik NC, Lim CS, Jang HS (2013) Numeric and morphological verification of lumbosacral segments in 8280 consecutive patients. Spine 38: 573-578.
- Tang M, Yang XF, Yang SW, Han P, Ma YM, et al. (2014) Lumbosacral transitional vertebra in a population-based study of 5860 individuals: prevalence and relationship to low back pain. Eur J Radiol 83: 1679- 1682.
- Luoma K, Vehmas T, Raininko R, Luukkonen R, Riihimäki H (2004) Lumbosacral transitional vertebra: relation to disc degeneration and low back pain. Spine 29: 200-205.
- Nardo L, Alizai H, Virayavanich W, Liu F, Hernandez A, et al. (2012) Lumbosacral transitional vertebrae: association with low back pain. Radiol 265: 497-503.
- Apazidis A, Ricart PA, Diefenbach CM, Spivak JM (2011) The prevalence of transitional vertebrae in the lumbar spine. Spine J 11: 858-862.
- Quinlan JF, Duke D, Eustace S (2006) Bertolotti’s syndrome: a cause of back pain in young people. J Bone Jt Surg 88: 1183-1186.
- Peterson CK, Bolton J, Hsu W, Wood A (2005) A cross-sectional study comparing pain and disability levels in patients with low back pain with and without transitional lumbosacral vertebrae. J Manipulative Physiol Ther 28: 570-574.
- Bonaiuti D, Faccenda I, Flores A (1997) Sacralization of the 5th lumbar vertebra and backache: what's the possible relationship?. La Medicina del lavoro 88: 226-236.
- Jancuska JM, Spivak JM, Bendo JA (2015) A review of symptomatic lumbosacral transitional vertebrae: Bertolotti's syndrome. Int J Spine Surg 9.
- Konin GP, Walz DM (2010) Lumbosacral transitional vertebrae: classification, imaging findings, and clinical relevance. Am J Neuroradiol 31: 1778-1786.
- Milicic G, Krolo I, Anticevic D, Roic G, Zadravec D (2012) Causal connection of non-specific low back pain and disc degeneration in children with transitional vertebra and/or spina bifida occulta: role of magnetic resonance–prospective study. Coll Antopol 36: 627-633.
- Connolly LP, d’Hemecourt PA, Connolly SA, Drubach LA, Micheli LJ, et al. (2003) Skeletal scintigraphy of young patients with low-back pain and a lumbosacral transitional vertebra. J Nucl Med 44: 909-914.
- Connolly LP, Drubach LA, Connolly SA, Treves ST (2004) Young athletes with low back pain: skeletal scintigraphy of conditions other than pars interarticularis stress. Clin nucl med 29: 689-693.
- Macedo RB, Coelho-e-Silva MJ, Sousa NF, Valente-dos-Santos J, Machado-Rodrigues AM, et al. (2015) Quality of life, school backpack weight, and nonspecific low back pain in children and adolescents?. J Pediatr 91: 263-269.
- Reitsma AM, Schuler TC, Hasz MW, Poelstra KA (2002) Surgical treatment of symptomatic Bertolotti's syndrome in post-fusion patients.
- Santavirta S, Tallroth K, Ylinen P, Suoranta H (1993) Surgical treatment of Bertolotti's syndrome. Arch Orthop Trauma Surg 112: 82-87.
- Brault JS, Smith J, Currier BL (2001) Partial lumbosacral transitional vertebra resection for contralateral facetogenic pain. Spine 26: 226-229.
- Aihara T, Takahashi K, Ogasawara A, Itadera E, Ono Y, et al. (2005) Intervertebral disc degeneration associated with lumbosacral transitional vertebrae: a clinical and anatomical study. J Bone Jt Surg 87: 687-691.
- Hashimoto M, Watanabe O, Hirano H (1996) Extraforaminal stenosis in the lumbosacral spine: efficacy of MR imaging in the coronal plane. Acta Radiol 37: 610-613.
- Otani K, Konno S, Kikuchi S (2001) Lumbosacral transitional vertebrae and nerve-root symptoms. J Bone Jt Surg 83: 1137-1140.
- Murtaugh K, Kean WF (2008) The clinical assessment of transitional vertebrae and back pain. Inflammopharmacology 16: 278-283.
- Tokgoz N, Ucar M, Erdogan AB, Kilic K, Ozcan C (2014) Are spinal or paraspinal anatomic markers helpful for vertebral numbering and diagnosing lumbosacral transitional vertebrae?. Korean J Radiol 15: 258-266.
- Farshad-Amacker NA, Lurie B, Herzog RJ, Farshad M (2014) Interreader and intermodality reliability of standard anteroposterior radiograph and magnetic resonance imaging in detection and classification of lumbosacral transitional vertebra. Spine J 14: 1470-1475.
- de Bruin F, Ter Horst S, Bloem JL, van den Berg R, de Hooge M, et al. (2017) Prevalence and clinical significance of lumbosacral transitional vertebra (LSTV) in a young back pain population with suspected axial spondyloarthritis: results of the SPondyloArthritis Caught Early (SPACE) cohort. Skeletal radiol 46: 633-639.
- Friedrich KM, Nemec S, Pelosche P, Pinker K, Weber M, et al. (2007) The prevalence of lumbar facet joint edema in patients with low back pain. Skeletal radiol 36: 755-760.
- Pekindil G, Sarikaya A, Pekindil Y, Gültekin A, Kokino S (2004) Lumbosacral transitional vertebral articulation: evaluation by planar and SPECT bone scintigraphy. Nucl med communications 25: 29-37.
- Marks RC, Thulbourne T (1991) Infiltration of anomalous lumbosacral articulations: steroid and anesthetic injections in 10 back-pain patients. Acta Orthop Scandinavica 62: 139-141.
- Li Y, Lubelski D, Abdullah KG, Mroz TE, Steinmetz MP (2014) Minimally invasive tubular resection of the anomalous transverse process in patients with Bertolotti's syndrome: presented at the 2013 Joint Spine Section Meeting. J Neurosurgery Spine 20: 283-290.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences