Multi-Level Lumbar Disc Replacements: Review of the Specificities and Difficulties of the Surgical Technique
Raphal Pietton,Jean-Charles Aurgan,Philippe Cottin and Thierry Begue
DOI10.21767/2471-8173.100001
Raphaël Pietton, Jean-Charles Aurégan*, Philippe Cottin and Thierry Bégué
Department of Orthopedic Surgery and Traumatology, Antoine Béclère Hospital, AP-HP, Paris Sud University, 157 rue de la Porte de Trivaux, 92140 Clamart, France
- *Corresponding Author:
- Jean-Charles Aurégan
Department of Orthopaedic Surgery and Traumatology, Antoine Béclère hospital, APHP, Paris Sud University, 157 rue de la Porte de Trivaux, 92140 Clamart, France
Tel: 01 45 37 49 38
Fax: 01 45 37 49 50
Email:aureganjc@yahoo.fr
Received date: July 15, 2015; Accepted date: September 28, 2015; Published date: October 03,2015
Abstract
Purpose: Lumbar disc replacement is a seducing therapeutic option to address the isolated discogenic disc disease in young patients. While of relatively recent creation, the technique of implantation of a single-level disc replacement is now widely disseminated. Because of promising results, it is now frequent to observe an increase of the number of lumbar discs replaced during a single procedure. Hence, several publications reported cases of lumbar disc replacements at two or three levels. However, we feel that multi-level lumbar disc replacements should not be approached as the sum of several one-level lumbar disc replacements. Methods: It seems interesting to highlight some aspects of the surgical technique of multi-level lumbar disc replacements in order to improve their implantation. In this study, we aimed to present the specificities and difficulties of the surgical technique for multi-level lumbar disc replacements. Results: First, we reviewed the common aspects of any lumbar disc replacement, then the specific points of the multi-level ones. Specific caution must be taken during the necessary wide surgical approach, especially with the vascular components, and with the sequence used to implant the different arthroplasties. Finally, a specific care must be taken to choose the adequate type of arthroplasty in order to equilibrate the lumbar lordosis, which will not be adjusted by the adjacent native discs. We illustrated these descriptions with clinical examples from our practice. Conclusion: multi-level lumbar disc replacements necessitate a specific surgical technique in order to optimize the implantation, to improve the results, and to reduce complications.
Introduction
Isolated discogenic disc disease is a major cause of chronic low back pain among young patients [1]. Despite its relatively important incidence, treatment has not been standardized yet [2]. Once the medical treatment is overwhelmed, for most of the authors, surgical options are divided between anterior and/ or posterior fusion techniques and lumbar disc replacement [3]. Due to its promising results, lumbar disc replacement is now recognized as a key component of surgical treatment of the discogenic disc disease in young patients [4].
On one hand, the surgical technique of a single-level lumbar disc replacement has been well documented now [5-7]. On another hand, because of promising results, it is now frequent to observe an increase of the number of lumbar discs replaced during a single procedure. Despite the seducing aspect of a single stage treatment for concomitant disc diseases, this is not without difficulties because we feel that multi-level lumbar disc replacements should not be approached as the sum of several one-level lumbar disc replacements. In fact, multi-level lumbar disc replacements necessitate a precise preoperative assessment and a demanding surgical procedure [4].
In this study, we aimed to present the specificities and difficulties of the surgical technique for multi-level lumbar disc replacements. First, we will review the common aspects of any lumbar disc replacement, then the specific points of the multi-level ones. Specific caution must be taken during the necessary wide surgical approach, especially with the vascular components, and with the sequence used to implant the different arthroplasties. Finally, a specific care must be taken to choose the adequate type of arthroplasty in order to equilibrate the lumbar lordosis, which will not be adjusted by the adjacent native discs. We will illustrate these descriptions with clinical examples from our practice.
Review of the specificities and difficulties of the surgical technique
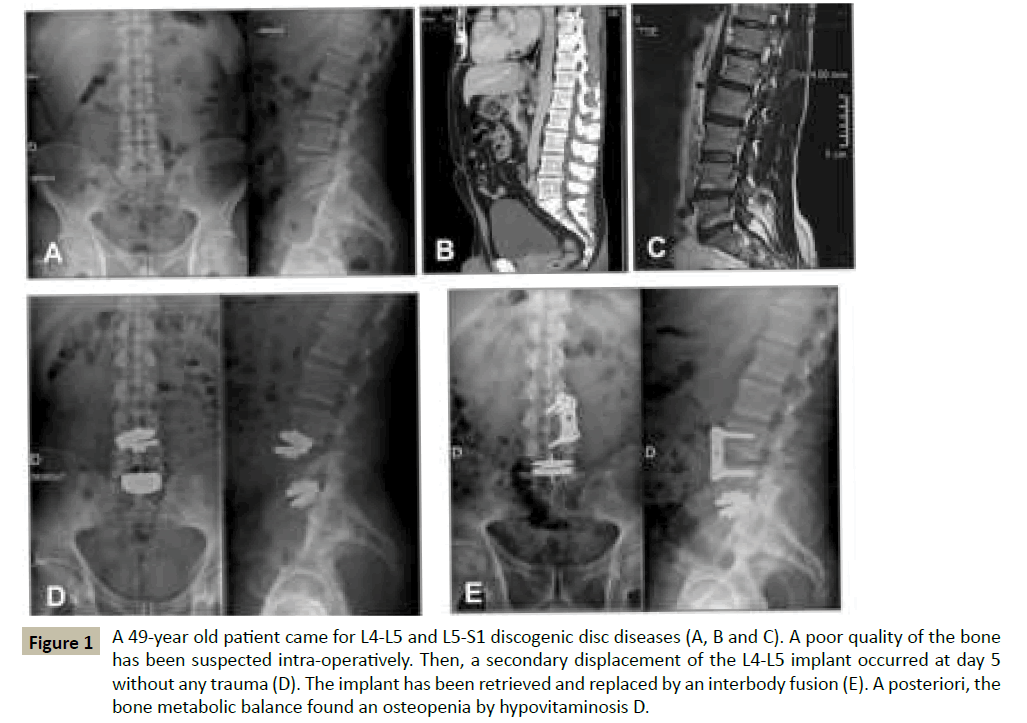
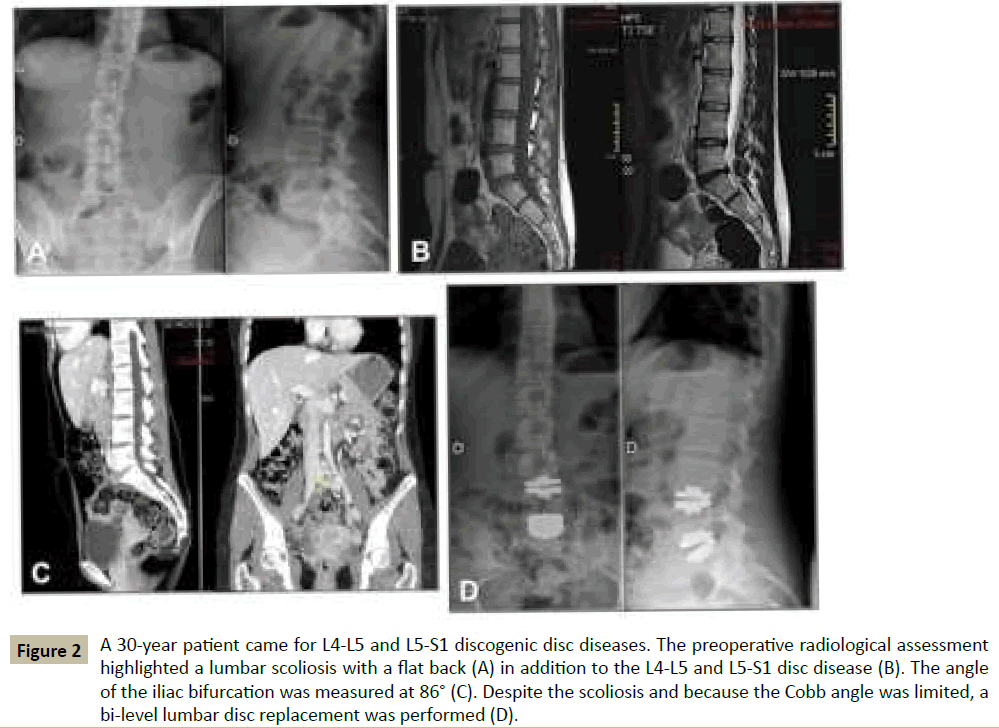
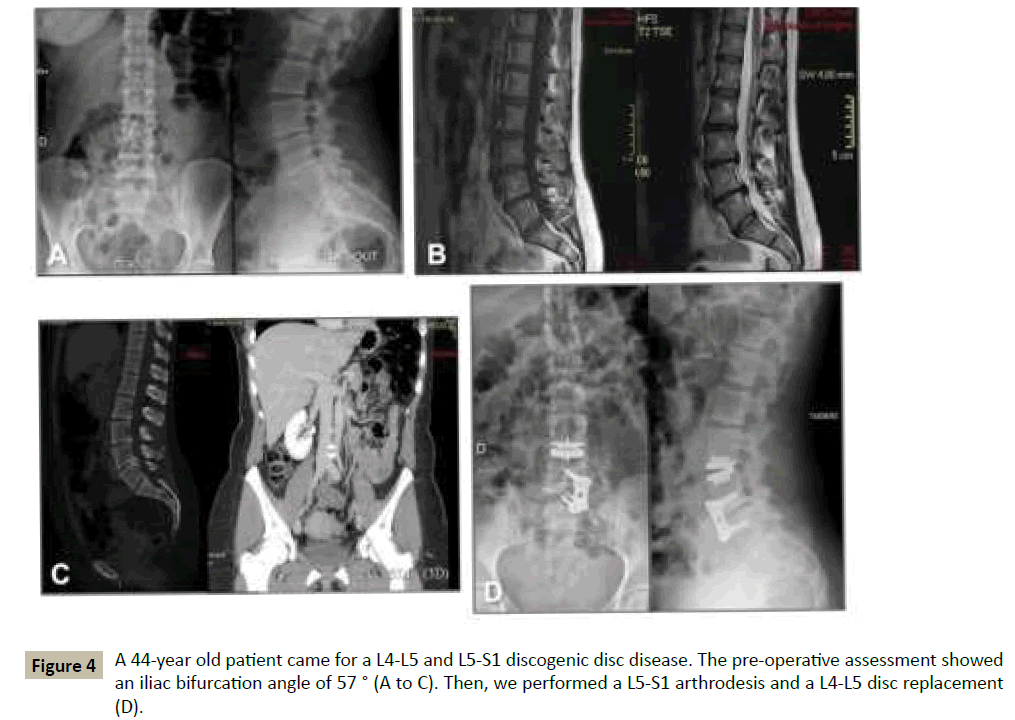
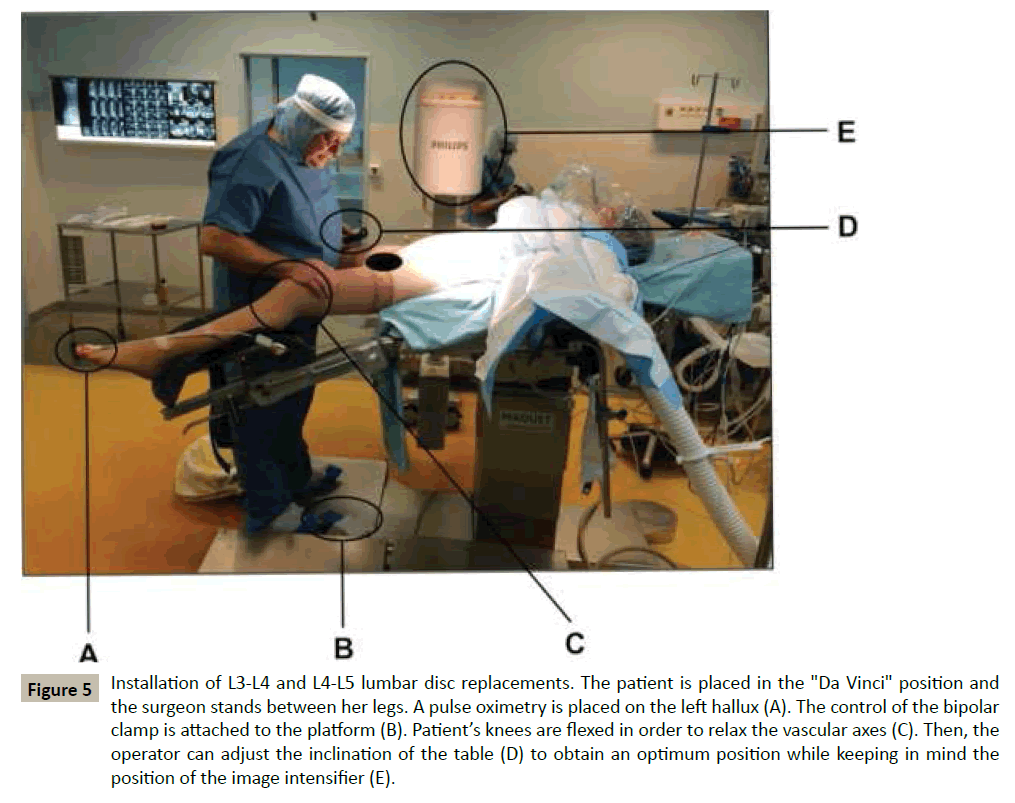
First, the clinical pre-operative assessment seeks to identify a strict contraindication to a disc replacement. We retain two of them mainly: an antecedent of spine infection or a previous spine surgery potentially destabilizing such as a laminectomy [6]. Then, the clinical pre-operative assessment seeks to evaluate the relative contraindications to a disc replacement. We retain several of them, which are elements that should prompt caution for implantation of prosthesis due to the risk of bone weakness: history of heavy smoking, early menopause, a longterm corticosteroid use [7-9]. For this specific problem, some recommended performing systematically a bone densitometry in women over 45 years in order to estimate the bone quality [9-11]. In fact, when a multi-level lumbar disc replacement is proposed, the notion of bone quality becomes paramount because the mechanical risk increases tenfold (Figure 1). Finally, we seek systematically any history of previous abdominal surgery in order to anticipate a possible difficulty to perform the anterior retroperitoneal approach [7]. Second, the pre-operative imaging assessment aims to identify cases where a disc replacement may be contra-indicated. We retain several of them: a destabilization in the frontal plane such as a scoliosis, a destabilization in the sagittal plane such as a spondylolisthesis, a lumbar spinal stenosis or a substantial facet arthrosis [7]. In case of a scoliosis, a Cobb angle greater than 20° (Figure 2) and/or an interbody angulation greater than 8° could represent a contraindication for lumbar disc replacement. Finally, the presence of an excessively oblique sagittal inter-somatic angle - especially at the L5-S1 level (Figure 3) – should be carefully considered [8]. This consideration is important in multi-level lumbar disc replacement because it could lead to an excessive stress on the implants at the L5-S1 level even if - to our knowledge - this is not demonstrated yet. Finally, we perform systematically a CT angiography - or a MRI angiography if CT angiography is not possible - to assess the anatomy of the iliac vessels, the presence of an iliolumbar vein, and both the height and angle of the vena cava confluence. Thus, from our experience, we consider that an angle greater than 50° (Figure 4) is a relative contraindication for lumbar disc replacement at the concerned level [12].
Figure 1 A 49-year old patient came for L4-L5 and L5-S1 discogenic disc diseases (A, B and C). A poor quality of the bone has been suspected intra-operatively. Then, a secondary displacement of the L4-L5 implant occurred at day 5 without any trauma (D). The implant has been retrieved and replaced by an interbody fusion (E). A posteriori, the bone metabolic balance found an osteopenia by hypovitaminosis D.
Figure 2 A 30-year patient came for L4-L5 and L5-S1 discogenic disc diseases. The preoperative radiological assessment highlighted a lumbar scoliosis with a flat back (A) in addition to the L4-L5 and L5-S1 disc disease (B). The angle of the iliac bifurcation was measured at 86° (C). Despite the scoliosis and because the Cobb angle was limited, a bi-level lumbar disc replacement was performed (D).
Figure 3 A 43-year old patient came for L3-L4, L4-L5 and L5-S1 discogenic disc diseases. The preoperative radiological assessment highlighted a sacral slope of 53°, a pelvic version of 26° and an incidence of 79°. It was decided to perform a L5-S1 arthrodesis plus L4-L5 and L3-L4 lumbar disc replacements.
Third, anesthesia and installation are identical regardless of the number of disc to address (Figure 5 and Appendix 1). Under general anesthesia, a Foley catheter is inserted to decompress the bladder and the patient is placed in a "Da Vinci" position: supine, arms and lower limbs abducted on gynecological supports, with the knees slightly flexed in order to relax the iliac axes. The surgeon stands between the patient's legs. A pulse oximetry is placed on the left hallux in order to detect an ischemia caused by the compression of the vessels with the retractors. Before the retraction of the vessels, the pulse oximetry should be equal to the pulse oximetry placed at the upper limb. During the retraction of the vessels, the pulse oximetry often decreases to zero and if the period of ischemia reaches 45 minutes, we release the retractors for ten minutes in order to perfuse the leg. Finally, the patient's curarization is highly recommended in order to reduce the intraabdominal pressure and so, the risk of peritoneal breach.
Figure 5 Installation of L3-L4 and L4-L5 lumbar disc replacements. The patient is placed in the "Da Vinci" position and the surgeon stands between her legs. A pulse oximetry is placed on the left hallux (A). The control of the bipolar clamp is attached to the platform (B). Patient’s knees are flexed in order to relax the vascular axes (C). Then, the operator can adjust the inclination of the table (D) to obtain an optimum position while keeping in mind the position of the image intensifier (E).
Fourth, we use an anterior and retroperitoneal approach to access the spine (Appendix 2). The skin incision is an oblique left paramedian incision, placed 2 cm from the midline and centered on the level previously identified by image intensifier. Its size depends on the patient's corpulence and the number of discs to replace. Usually, the size of an incision is 8 cm for one level, 12 cm for two and 15 cm for three. The first disc to approach depends on the number of levels to replace. In our experience, the L5-S1 space is the easiest to deal with after a retroperitoneal approach. The disc is located just below the aortic bifurcation and the left iliac vein covers the left side of the disc. Thus, it should be mobilized laterally and proximally with gentle maneuvers. First, the presacral vessels must be identified and ligated. The use of electrocautery is prohibited given the proximity of the hypogastric plexus and surgical clips should be preferred. Then, we think that the L4-L5 space is more difficult to approach. Indeed, it seems that the peritoneum facing this level is more fragile and thus, we cut the Douglas arcade and we approach the disc with a manual dissection. The iliac vessels cover the front of the disc and we mobilize them gradually from the left to the right. Care must be taken to identify any iliolumbar vein at this level. Its presence is usually suspected on the preoperative imaging but it is not uncommon to find an iliolumbar vessel during the procedure with a normal angiography scanner. Finally, it is important to keep in mind that oblique prostheses have been developed to ease the insertion of an implant when only the left half of the disc surface is available [12]. Finally, once the L4-L5 space has been approached, the extension to the upper level is easier. The L3-L4 space is located above the aortic bifurcation and care should be taken to ligate the segmental vessels for the spine. The surgical space is now prepared and the prostheses can be implanted safely.
During the implantation of multi-level lumbar disc replacements, we recommend to start the implantations at the lowest level and then, to proceed up to the overlying levels. The reason is to progress from a fixed point from which we can "build" the stepped disc recovery. The preparation and the distraction of the disc spaces during a multi-level lumbar disc replacement do not differ from a single-level disc replacement. In the same way, testing the implant sizes and implanting the final prostheses are the same as if the replacement was carried out at one or more levels. However, the lumbar lordosis should be carefully anticipated preoperatively to allow an optimal mobility in flexion - extension [13]. Furthermore, when using oblique prostheses -often at the L4-L5 level - any lateralization of an implant should be carefully avoided because it would result in an excessive stress on the adjacent implants. As postoperative recommendations, we allow the full weight bearing the day after the procedure without restraint regardless of the number of levels replaced. However, we forbid extreme movements in flexion or extension during six weeks postoperatively. Finally, we recommend the use of compression socks and a pharmacological thromboprophylaxis for a period of 30 postoperative days. In addition, we always perform a venous Doppler ultrasound of the lower limbs on the fifth postoperative day to detect any subclinical deep thrombophlebitis.
Discussion
Despite the seducing aspect of a single stage treatment for concomitant disc diseases, multi level lumbar disc replacements are not without difficulties because we feel that they should not be approached as the sum of several one-level lumbar disc replacements. In fact, multi-level lumbar disc replacements necessitate a precise preoperative assessment and a demanding surgical procedure [4].
Even if the impact of low back pain in young patients seems important, it is difficult to assess the proportion of patients in whom a multi-level lumbar disc replacement could be proposed.
Based on the epidemiological studies of discogenic disc disease, the number of multi-level diseases - and therefore potentially multi-level disc replacements - is low. In fact, Siepe et al. reported 18,3% of bi-prostheses - first at L4-L5-S1 (17,2%) then at L3-L4-L5 (1,1%) - on 93 patients during a period going from 1991 to 2003 [8].
The anatomical, functional and mechanical results of the multilevel lumbar disc replacements are difficult to assess. In fact, several studies reporting the results of lumbar disc replacement in general displayed a certain proportion of their population with 2 to 3 levels replaced. However, even if the functional outcomes seem very good with a short-term follow-up, the duration of the implant and eventual premature failure are not known [14].
In conclusion, lumbar disc replacements for discogenic disc disease of young patients are trending toward a standardization of the procedure and a simplification of the process. That would probably make the bed of an increase in the number of multilevel replacements proposed. At term, it seems that the challenge will be to optimize the implant survival although the mechanical loosening and / or wear observed are very rare so far.
Conflict of Interest
The authors certify that they have no financial conflict of interest (eg, consultancies, stock ownership, equity interest, patent/ licensing arrangements, etc) in connection with this article.
References
- Kjaer P, LeboeufYC, Korsholm L, Sorensen JS, Bendix T (2005) Magnetic resonance imaging and low back pain in adults: a diagnosis Imaging study of 40-year-old men and women. Spine 30:1173-1180.
- Modic MT, Masaryk TJ, Ross JS, Carter JR (1988) Imaging of degenerative disk disease. Radiology 168:177-186.
- Karppinen J, Shen FH, Luk KD, Andersson GB, Cheung KM, et al. (2011) Management of degenerative disk disease and chronic low back pain. OrthopClin North Am 42:513-528.
- Bertagnoli R. Kumar S (2002) Indications for full prosthetic disc arthroplasty: a correlation of clinical outcome against a variety of indications. Eur Spine J 11:S131-136.
- Zigler J, Delamarter R, Spivak JM, LinovitzRJ, Danielson G, et al. (2007) Results of the prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of the ProDisc-L total disc replacement versus circumferential fusion for the treatment of 1-level degenerative disc disease. Spine (Phila Pa 1976) 32:1155-1162.
- Tropiano P, Huang RC, Girardi FP, Cammisa FP Jr, Marnay T (2006) Lumbar total disc replacement - Surgical technique. J Bone Joint Surg Am 88:50-64.
- Huang RC, Lim MR, Girardi FP, Cammisa FP Jr (2004) The prevalence of contraindications to total disc replacement in a cohort of lumbar surgical patients. Spine (Phila Pa 1976) 29: 2538-2541.
- Siepe CJ, Zelenkov P, Sauri-Barraza JC, Szeimies U, Grubinger T, et al. (2010) The fate of facet joint and adjacent level disc degeneration following total lumbar disc replacement: a prospective clinical, X-ray, and magnetic resonance imaging investigation. Spine (Phila Pa 1976) 35: 1991-2003.
- Baur-Melnyk A, Birkenmaier C, Reiser MF (2006) Lumbar disc arthroplasty: indications, biomechanics, types, and radiological criteria. Radiologe 46: 770-778.
- Gerometta A, Rodriguez Olaverri JC, Bittan F (2012) Infection and revision strategies in total disc arthroplasty. IntOrthop 36: 471-474.
- Strube P, Hoff EK, Perka CF, Gross C, Putzier M (2012) Influence of the Type of the Sagittal Profile on Clinical Results of Lumbar Total Disc Replacement After a Mean Follow-up of 39 Month. J Spinal Disord Tech, Epub ahead of print, PMID: 23222097.
- Diesinger Y, Charles YP, Bouaka D, Godet J, Steib JP (2012) Preoperative phlebography in anterior L4-L5 disc approach - Clinical experience about 63 cases. OrthopTraumatolSurg Res 98:887-893.
- Schmidt H, Galbusera F, Rohlmann A, Zander T, Wilke HJ (2012) Effect of multilevel lumbar disc arthroplasty on spine kinematics and facet joint loads in flexion and extension a finite element analysis. Eur Spine J 21:S663-674.
- Hannibal M, Thomas DJ, Low J, Hsu KY, Zucherman J (2007) ProDisc-L total disc replacement a comparison of 1-level versus 2-level arthroplasty patients with a minimum 2-year follow-up. Spine (Phila Pa 1976) 32:2322-2326.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences