Peri-Radicular Fibrosis After Lumbar Surgery: Is There Any Help?
Inaki Arrotegui
DOI10.21767/2471-8173.100002
Iñaki Arrotegui*
Department of Neurosurgery, Valencia University General Hospital, Valencia (Spain)
- *Corresponding Author:
- Dr. Iñaki Arrotegui
Consultant Neurosurgeon, Valencia University General Hospital, Department of Neurosurgery, Avda. Tres Cruces s/n, 46014– Valencia (Spain)
Tel: 0034627492961
Email:athbio@yahoo.es
Received date: August 27, 2015; Accepted date: September 21, 2015; Published date: September 24,2015
Abstract
Study Design: This study was based on Clinical Trial medical records from the Valencia University General Hospital (Hospital General Universitario de Valencia), Spain. The study population consisted of patients who underwent spinal surgery and who had documented follow-up visits for at least 2 years afterwards.
Background
Peridural fibrosis is the scar tissue formed over the dura mater after a laminectomy. It has been implicated as a cause of the persistence of pain after spinal surgery and associated with an increased risk of complications during revision surgery [1,2]. The application of a mechanical barrier to cover the peridural space to block the migration of inflammatory cells from superficial layers to the epidural space can, potentially, prevent or decrease scar formation [3]. The authors evaluated the use of SuproFilm for this purpose.
Postoperative fibrosis is one of the most important causes of Failed Back Surgery Syndrome after lumbar disc surgery [4]. Numerous natural and synthetic materials have been investigated as a means to prevent or reduce postoperative scarring after these operations.
A retrospective clinical study was conducted. The aim was to present a new idea during lumbar discectomy, and to evaluate whether this helps to prevent or diminish postoperative fibrosis. Peridural fibrosis that develops after lumbar discectomy may be responsible for as much as 20% of all cases of Failed Back Surgery Syndrome. A variety of biological and non-biological materials have been used as a barrier against the invasion of fibrous tissue into the vertebral canal.
The purpose of this study was to evaluate the use of SL Matrix to inhibit peridural fibrosis and reduce FBSS symptoms after lumbar discectomy.
SL is a transparent, flexible, cuttable, does not stick to the glove, is easy to apply, it has its own bonding agent, which means that no suture is required. SL is an anti-adhesive membrane for the prevention of postoperative adhesions. SLM is applied directly on the wound surface forming a sticky liquid from the first day. It prevents the wound surface from starting to absorb glucosamine monomer liquid from the film thus increasing the repair and renovation of the serum layer. It has a characteristic that limits fibroblasts which cause hyperplasy. It decreases the formation of collagen and saves collagen fibre groups. It does not affect the formation of collagen and wound healing.
Observations on fibrosis
The extent of fibrosis varies from patient to patient, depending on the inflammatory response, vascular condition, and surgical approach/technique.
The development of an effective barrier for the inhibition of postsurgical fibrosis is critical to achieving an optimal clinical result.
The objective of this prospective clinical study was to investigate the potential benefits of using the SL Matrix as an adhesion barrier following spine surgery in order to avoid peri-radicular lumbar fibrosis
Material and Methods
Prospective Review of 200 patients 2010-2013
Control Group 100
DuraGen Group 100
Surgery of the lumbar spine
Follow up for a minimum of two years
Clinical follow up
1 month, 3 months, 6 months, 1-4 years
Post-operative Pain Assessment at each time point:
2 = No Pain, 3 = Mild Pain, 4 = Moderate Pain, 5 = Severe Pain
Extent of Fibrosis graded by Gad-MRI:
In a prospective study we compared postoperative results of 100 patients who had a Dural Graft matrix implanted during lumbar discectomy with the results obtained from 100 patients in whom no material was implanted. The outcomes were evaluated using a questionnaire on activities of daily living according to the Low Back Outcome Score, pain-grading scale.
Results
Pain Outcomes: Results from the Control Group (Standard Practice)
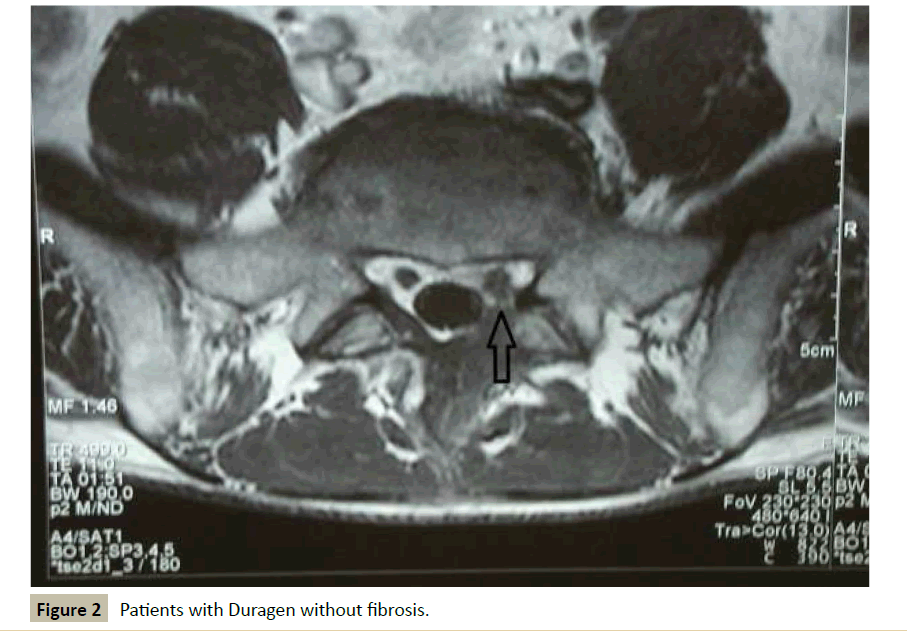
Patients with more fibrosis, shown by the arrows, exhibited more significant symptoms Figure 1.
Results from the SL Group Figure 2.
Postsurgical fibrosis was found in 2% of the Collagen Group vs 8% in the Control G
MRI image of fibrosis after surgery Figures 1 and 2.
Mean postoperative pain scores for the SL Group were lower at all time points and statistically lower at 3 to 6 months.
None of the 100 patients from the SL Group required re-operation for symptoms due to fibrosis.
The difference in re-operation rate between the SL group and the standard procedure group is statistically significant (p<0.01).
Discussion
There is a need for treatments that prevent dural adhesions and minimize the impact of peridural fibrosis on the post-operative outcome of spine surgery [5-7].
The development of postoperative scar tissue and adhesions is a natural consequence of healing, but can be associated with general medical and reoperation complications. Many biocompatible products have been evaluated as barriers or deterrents to adhesions [8-10].
The failed back surgery syndrome (FBSS) is a severe, longlasting, disabling and relatively frequent (5-20%) complication of lumbosacral spine surgery [11,12]. The wrong level of surgery, inadequate surgical techniques, vertebral instability, recurrent disc herniation, and lumbo-sacral fibrosis are the most frequent causes of FBSS [13,14].
Approximately 15% of all laminectomy or discectomy patients experience persistent disabling pain in the hip, thigh, leg, or lower back. These symptoms have been linked to peridural scarring (fibrosis), spinal stenosis, retained disc fragments, and other surgical complications, such as pseudoarthrosis and infection [15]. Peridural fibrosis can bind the dura and nerve roots leading to persistent sciatic and lumbar pain, which may require reoperation [16,17].
Given the link between peridural fibrosis and costly re-operation, a considerable amount of effort has gone into the development of techniques and materials to prevent epidural adhesions. The results, after repeated surgery on recurrent disc herniations, are comparable to those after the first intervention, whereas repeated surgery for fibrosis gives only a 30-35% success rate, and 15-20% of the patients report worsening of the symptoms [18,19]. Computerized tomography (CT) with contrast medium and, in particular, Gd-DPTA enhanced MRI have allowed a differentiation between these two pathologies permitting us to adopt different therapies [20].
In a comparison between spinal surgery patients undergoing anti-adhesion treatment with either SLG or Standard Procedure, the percentages of patients requiring re-operation were approximately 2% SLG and 8% Standard.
After a period of approximately two years of follow-up, later reoperation began to lean heavily in favour of SL.
When categorized by diagnosis (most commonly Ruptured Disc and Stenosis), the results consistently favoured the SLG vs Standard Procedure.
In addition, the SLG group consistently exhibited less pain and fewer adhesions during follow-up.
The two treatment groups were similar with regard to demographic characteristics and, in general, as regard surgical characteristics.
Diagnoses were roughly divided into a 60% of Ruptured Disc:40% Stenosis in the SLG group while the corresponding division was about 80%:20% in the Standard group. However, this did not seem to have any effect on the superior response with SLG. Also, the SLG group had relatively more Lumbar L4-L5 cases and relatively fewer Single Level procedures than the Standard group, but this may not have been clinically important when making a comparison between the two treatment groups.
Conclusions
1. The data strongly suggest that treatment with SL Matrix was significantly more beneficial than treatment without an adhesion barrier in lumbar surgery patients. By preventing dural adhesions, the SL Matrix significantly reduced the need for re-operation to relieve recurrent pain.
2. The use of SL membrane improves the outcome of the surgical treatment of lumbar Spine Surgery.
References
- de Tribolet N, Porchet F, Lutz TW, Gratzl O, Brotchi J (1998) Clinical assessment of a novel antiadhesion barrier gel: prospective, randomized, multicenter, clinical trial of ADCON-L to inhibit postoperative peridural fibrosis and related symptoms after lumbar discectomy. Am J Orthop 27:111-120.
- Geisler FH (1999) Prevention of peridural fibrosis: current methodologies. Neurol Res 21 Suppl 1: S9-S22.
- Long DM (1991) Failed back surgery syndrome. Neurosurg Clin No Am 2:899-19.
- Narotam PK, van Dellen JR, Bhoola KE, Raidoo D (1993) Experimental evaluation of collagen sponges as a dural graft. Br J Neurosurg 7:635-641.
- Narotam PK, van Dellen JR, Bhoola KD (1995) A clinicopathological study of collagen sponge as a dural graft in neurosurgery. J Neurosurg 82: 406-412.
- Narotam PK, Gousseau A, McGinn G, Use of Collagen Matrix (DuraGen) for DuraPlasty in Neurosurgery, presented at the Congress of Neurological Surgeons Annual Meeting, San Antonio TX, September.
- Pradeep K, Sunil J, Naren N, Taylon C, Vora Y, et al. (2003) The Role of Collagen Matrix (DuraGen@) tor Dural Repair Following Spinal Durotomy: Technique Appraisal and Clinical Review - presented at World Spine II: The Second Interdisciplinary Congress on Spine Care.
- Robertson JT (1996) Role of peridural fibrosis in the failed back: a review. Eur Spine 1:S2-S6
- Peace, Karl E (1988) Biopharmaceutical Statistics for Drug Development. Marcel Dekker: 403-420
- Khorasani L, Kapur RP, Lee C, Avellino AM (2008) Histological analysis of DuraGen in a human subject: case report. Clin Neuropathol 27: 361-364.
- 11 Tatsui CE, Martinez G, Li X, Pattany P, Levi AD (2006) Evaluation of DuraGen in preventing peridural fibrosis in rabbits. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2005. J Neurosurg Spine 4: 51-59
- Akeson WH, Massie JB, Huang B, Giurea A, Sah R, et al. (2005) Topical high-molecular-weight hyaluronan and a roofing barrier sheet equally inhibit postlaminectomy fibrosis. Spine J. 5: 180-190.
- Massie JB, Schimizzi AL, Huang B, Kim CW, Garfin SR,et al. (2005) Topical high molecular weight hyaluronan reduces radicular pain post laminectomy in a rat model. Spine J 5:494-502
- Hayashi S, Takayama T, Masuda H, Kochi M, Ishii Y, et al. (2008) Bioresorbable membrane to reduce postoperative small bowel obstruction in patients with gastric cancer: a randomized clinical trial. Ann Surg 247: 766-770.
- Zeng Q, Yu Z, You J, Zhang Q (2007) Efficacy and safety of Seprafilm for preventing postoperative abdominal adhesion: systematic review and meta-analysis. World J Surg 31 :2125-2131
- Khan WS, Tew SR, Adesida AB, Hardingham TE (2008) Human infrapatellar fat pad-derived stem cells express the pericyte marker 3G5 and show enhanced chondrogenesis after expansion in fibroblast growth factor-2. Arthritis Res Ther 10: 74
- Kayaoglu HA, Ozkan N, Hazinedaroglu SM, Ersoy OF, Koseoglu RD (2005) An assessment of the effects of two types of bioresorbable barriers to prevent postoperative intra-abdominal adhesions in rats. Surg Today 35: 946-950.
- Kanamori M, Kawaguchi Y, Ohmori K, Kimura T, Tsuji H, et al. (2001) The fate of autogenous free-fat grafts after posterior lumbar surgery: part 2. Magnetic resonance imaging and histologic studies in repeated surgery cases. Spine 26: 2264-2270.
- Alkay RN, KIM DH (2003) Prevention of postlaminectomy epidural fibrosis using bioelastic materials. Spine 28: 1659-1665.
- Ivanic GM, Pink PT, Schneider F, Stuecker M, Homann NC, et al. (2006) Prevention of epidural scarring after microdiscectomy: a randomized clinical trial comparing gel and expanded polytetrafluoroethylene membrane. Eur Spine J 15: 1360-1366.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences