Percutaneous Radiofrequency Ablation of a C2 Osteoblastoma
Chakraverty J, Grainger M, Da Silva EJ and James SLJ
DOI10.21767/2471-8173.100023
Chakraverty J1*, Grainger M2, Da Silva EJ2 and James SLJ2
1University Hospitals of Bristol NHS Foundation Trust, UK
2Royal Orthopaedic Hospital NHS Foundation Trust, UK
- *Corresponding Author:
- Chakraverty J
University Hospitals Bristol NHS Foundation Trust, Bristol, UK.
E-mail: jchakraverty@doctors.org.uk
Received date: December 29, 2016; Accepted date: February 28, 2017; Published date: February 06, 2017
Citation: Chakraverty J, Grainger M, Da Silva EJ, et al. Percutaneous Radiofrequency Ablation of a C2 Osteoblastoma. Spine Res. 2016, 3:1. doi: 10.21767/2471-8173.10001
Abstract
Cervical osteoblastoma is usually treated by marginal or en bloc surgical resection. There is however emerging evidence to support the use of a minimally invasive radiofrequency ablation (RFA) procedure which can be performed percutaneously.
Keywords
Minimally-invasive; Radiofrequency ablation; Osteoblastoma
Introduction
Jaffe first described osteoblastoma as pathologically distinct from osteoid osteoma in 1956 [1]. Although histologically similar, osteoid osteoma and osteoblastoma are frequently distinguished by size, with lesions less than 1.5 cm classified as the former and those larger than 1.5 cm the latter [2]. Osteoblastoma accounts for approximately 1% of all primary bone tumours and 3% of all benign bone tumours [3]. Although the long bones can be involved, it has a greater propensity to involve the spine. It tends to be more locally aggressive than osteoid osteoma and frequently can be seen to erode the bony cortex forming an associated expansile soft tissue mass. Radiofrequency ablation is considered the treatment of choice for the treatment of osteoid osteomas and osteoblastomas especially in the appendicular skeleton [4]. There is emerging evidence also to support its use in the spine [5]. We report a case of C2 osteoblastoma which was successfully managed with CT guided RFA.
Case Presentation
History and examination
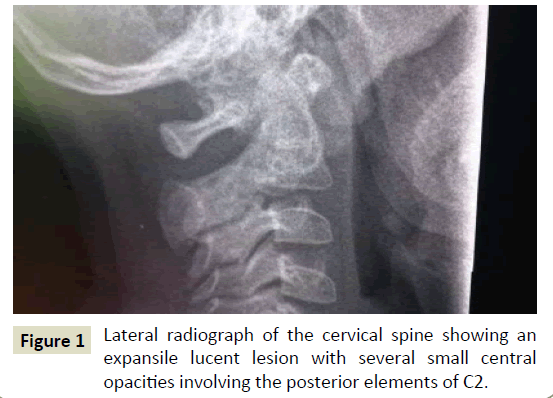
A 4-year-old girl presented with persistent neck pain and stiffness and difficulty with sleeping due to nocturnal pain. No systemic symptoms were reported. The initial examination revealed that the patient looked pale. She was afebrile. No postural abnormality was identified. She was focally tender on palpation of the upper cervical spine but range of motion of the cervical spine was considered normal. Neurological and abdominal examination was unremarkable with no evidence of hepatosplenomegaly. There was no lymphadenopathy. Blood tests revealed no abnormality; the full blood and white cell counts and C-reactive protein levels were all within the normal range. The initial diagnostic imaging included conventional radiography and MRI. A lateral radiograph of the cervical spine (Figure 1) revealed an expansile lucent lesion with several small centrals opacities involving the posterior elements of C2. MRI scan of the cervical spine (Figure 2) demonstrated an expansile lesion involving the lamina of C2 on the right side. The lesion demonstrated diffuse high signal on the T2 weighted and on the proton density fat saturated (Figure 2) imaging. Post i.v. injection with Gadolinium there was diffuse enhancement of the expansile lesion. Right sided enhancement of the C2 paravertebral region was also noted, but there was no evidence of a paravertebral soft tissue mass or collection. The differential diagnosis included osteoblastoma and infection although the presence of normal blood parameters favoured the former diagnosis.
Biopsy and pathological findings
Following discussion at a Spinal Oncology multi-disciplinary meeting a CT guided biopsy was performed. Subsequent histology revealed fragments of irregular woven bone lined by plump osteoblasts within a densely-vascularized stroma consistent with a diagnosis of osteoblastoma (Figure 3). Interestingly, the patient had noticed a significant reduction of pain following the biopsy although this may have been due to the concurrent prescription of indomethacin. Considering this, it was decided to treat the patient non-operatively with follow up imaging undertaken at 3 months. At that time, there had been an increase in pain and a progressive scoliotic deformity was evident clinically. There was extensive discussion between the family, spinal oncology team, paediatric spinal deformity team and interventional radiology team as to differing treatment options.
Interventional radiology
The patient subsequently underwent percutaneous RFA of the lesion under CT guidance. The intra-operative CT scan (Figure 4) showed a 2cm expansile lesion with central opacities in the lamina of C2 on the right side just lying posterior to the vertebral artery within the right foramen transversarium. The patient was placed in the prone position under full general anaesthesia. A mid-line approach was made using a Bonopty biopsy needle (14-gauge cannula, 16-gauge trephine needle; Radi Medical Systems, Uppsala, Sweden). The needle track was passed obliquely to extend away from the central spinal canal. Final needle position was checked using the axial, coronal and sagittal CT images. The 10 mm exposed tip of the RFA electrode was cited in the anterior aspect of the right C2 lamina and 5 mm away from the right vertebral artery (Figure 5 and 6). The medial cortex of the lamina remained intact. The lesion was then ablated (1 cycle, 90°C for 6 minutes).
Post-operative course
The patient underwent planned admission to the High Dependency Unit. The post-operative course was uneventful and the patient was discharged the following day. On the 2-week follow-up, the patient was pain free. At 3 months, analgesia was stopped with no recurrence of painful symptoms. At 12 months, the patient was symptom free and had returned to normal activities and was discharged from clinical review.
Discussion
Technical success and a positive outcome were achieved in our patient following CT guided percutaneous RFA. To our knowledge this case represents the first reported case of C2 osteoblastoma treated using this minimally invasive procedure. CT guided percutaneous RFA is a minimally invasive procedure and was first described as an option for the treatment of osteoid osteoma in 1992 by Rosenthal and co-workers [6]. An electrode is placed into the lesion and an alternating radiofrequency current is emitted by a generator. The electric current produces a focal thermal injury in tumour tissues leading to irreversible coagulative necrosis [7]. Its application for spinal osteoid osteoma was first reported by Osti et al. [8] and indeed is now considered the gold standard treatment for this primary bone tumour [5]. The case for spinal osteoblastoma RFA is less well established. Rehnitz et al. have reported on the long-term outcomes of CT guided RFA in 12 patients with osteoblastoma, and although their study involved treatment of lesions in critical locations, it is not clear if any of these lesions involved the spine [8,9].
The major concern with the use of RFA in the spine is the potential for thermal damage to the spinal cord and nerve roots. The lesion in our patient did not breach the cortex and it was therefore, felt the neural elements would be insulated from focal increases in temperature. This has certainly been shown to be the case in ex vivo studies [10]. Insufflation of air in the epidural space may also provide a cooling effect during the RFA procedure [11]. We did not use epidural cooling in our patient primarily because of the intact cortex. However, in other cases of spinal RFA performed in our institution, we have found that air preferentially fills the contralateral side of the epidural space suggesting that this may be of questionable value. This may be due to secondary inflammatory change within the epidural space on the ipsilateral side of the lesion.
Vanderschueren et al. indicated that a safety margin of greater than 2 mm between the tumour margin and the intraspinal structures is required to prevent thermal injury to the neural elements from RFA [12]. This same principle was applied to the right vertebral artery in our patient which was located 5 mm away from the electrode tip.
Previous reports have suggested marginal or en bloc resection as the treatment of choice in osteoblastoma [13-17]. Potential drawbacks to surgical intervention include instability and loss of cervical sagittal balance secondary to resection of posterior elements. In this age group, there is also the concern the surgical approach could result in an unplanned fusion potentially leading to subsequent deformity. If open surgery had been undertaken it is possible that instrumented fusion would need to be considered if a partial or complete facet joint resection was undertaken. Spinal cord and nerve injury has also been reported [18,19]. Furthermore, due to the hyper vascular nature of the osteoblastoma, embolization may also be required before surgery [20]. Radiotherapy has also been suggested as an option in cases where a complete surgical tumour resection is not possible. However, sarcomatous transformation is a recognised complication of this type of intervention [21].
Conclusion
Even though the cervical spine represents a technically challenging localisation for RFA, this case illustrates that this minimally invasive procedure could be considered as a first line option for cervical osteoblastoma but further research into this is required. The major advantage is in the maintenance of segmental spinal stability and rapid convalescence with minimal morbidity. A short hospital stay also makes RFA for spinal osteoblastoma an attractive and more cost-effective option than surgery.
References
- Jaffe HL (1956) Benign osteoblastoma. Bull Hosp Jt Dis 17: 141-151.
- Lucas DR (2010) Osteoblastoma. Arch Pathol Lab Med 134: 1460-1466.
- Haeley HJ, Ghelman B (1986) Osteoid osteoma and osteoblastoma. Clin Orthop Relat Res 204: 76-85.
- Zouari L, Bousson V, Hamze B, Roulot E, Roqueplan F, et al. (2008) CT-guided percutaneous laser photo-coagulation of osteoid osteomas of the hands and feet. Eur Radiol18: 2635-2641.
- Martel J, Bueno A, Nieto-Morales ML, Ortiz EJ (2009) Osteoid osteoma of the spine: CT guided 569. Eur J Radiol 71: 564-569.
- Rosenthal DI, Alexander A, Rosenberg AE, Springfield D (1992) Ablation of osteoid osteomas with a percutaneously placed electrode: A new procedure. Radiology 183: 29-33.
- Gangi A, Basile A, Buy X, Alizadeh H, Sauer B, et al. (2005) Radiofrequency and laser ablation of spinal lesions. Seminars in Ultrasound, CT and MRI 26: 89-97.
- Osti OL, Sebben R (1998) High-frequency radio-wave ablation of osteoid osteoma in the lumbar spine. Eur Spine J 7: 422-425.
- Rehnitz C, Sprengel SD, Lehner B, Ludwig K, Omlor G, et al. (2012) CT-guided radiofrequency ablation of osteoid osteoma and osteoblastoma: Clinical success and longterm follow up in 77 patients. Eur J Radiol 81: 3426-3434.
- Dupuy DE, Hong R, Oliver B, Goldberg SN (2000) Radiofrequency ablation of spinal tumors: Temperature distribution in the spinal canal. Am J Roentgenol 175: 1263-1266.
- Rybak LD, Gangi A, Buy X, La Rocca Viera R, Wittig J (2010) Thermal ablation of spinal osteoid osteomas close to neural elements: Technical considerations. Am J Roentgenol 195: 293-298.
- Vanderschueren GM, Obermann WR, Dijkstra SP, Taminiau AH, Bloem JL, et al. (2000) Radiofrequency ablation of spinal osteoid osteoma: Clinical outcome. Spine 34: 901-904.
- Li Z, Zhao Y, Hou S, Mao N, Yu S, et al. (2013) Clinical features and surgical management of spinal osteoblastoma: A retrospective study in 18 cases. PLoS One 8(9): e74635.
- Kaner T, Sasani M, Oktenoglu T, Aydin S, Ozer AF (2010) Osteoid osteoma and osteoblastoma of the cervical spine: The cause of unusual persistent neck pain. Pain Physician 13: 549-554.
- 15. Kandziora F, Pingel A (2010) Posterior-anterior resection of a cervical spine osteoblastoma. Eur Spine J 19: 1041-1043.
- Rajasekaran S, Kanna RM, Kamath V, Shetty AP (2010) Computer navigation-guided excision of cervical osteoblastoma. Eur Spine J 19: 1046-1047.
- Charles YP, Schuller S, Sfeir G, Steib JP (2014) Cervical osteoblastoma resection and posterior fusion. Eur Spine J 23: 711-712.
- Faraj A, Byrne P, Mehdian H (1998) Osteoid osteoma of the lateral mass of C5 should excision be combined with fusion? Eur Spine J 7: 242-245.
- Laus M, Albisinni U, Alfonso C, Zappoli FA (2007) Osteoid osteoma of the cervical spine: Surgical treatment or percutaneous radiofrequency coagulation? Eur Spine J 16: 2078-82.
- Yilmaz C, Civelek E, Caner H, Aydin E, Gerilmez A, et al. (2012) Osteoblastoma of C2 corpus: 4 years follow-up. Asian Spine J 6: 136-139.
- Stavridis SI, Pingel A, Schnake KJ, Kandziora F (2013) Diagnosis and treatment of a C2-osteoblastoma encompassing the vertebral artery. Eur Spine J 22: 2504-2512.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences