Morphometrical and Clinical Analysis of Cervical Nucleoplasty Cases Using Coblation Technique
Hamit Selim Karabekir,Elmas Atar, Ahmet Yildizhan, Ayse Canan Yazici,Nilufer Demirci Yonguc,and Nuket Gocmen Mas5
DOI10.21767/2471-8173.100021
1Dokuz Eylul University School of Medicine, Turkey
2Istanbul Spinal Surgery Center, Turkey
3Neurosurgery Department, Yeditepe University School of Medicine, Izmir University, Turkey
4Department of Biostatistics, School of Medicine, Turkey
5Department of Anatomy, Dokuz Eylul University School of Medicine, Turkey
- *Corresponding Author:
- Selim Karabekir H
MD, Asc. Prof., Neurosurgery Department, Dokuz Eylul University School of Medicine, Izmir, Turkey.
E-mail: hskarabekir@hotmail.com
Received date: June 07, 2016; Accepted date: April 20, 2017; Published date: April 25, 2017
Citation: Karabekir HS, Atar E, Yildizhan A, et al. Morphometrical and Clinical Analysis of Cervical Nucleoplasty Cases Using Coblation Technique. Spine Res. 2017, 3:1.
Abstract
Background: Nucleoplasty is a minimally invasive procedure for managing chronic discogenic cervical pain. We aimed to evaluate the outcomes of nucleoplasty treatment on chronic cervical discogenic pain, intervertebral disc volumetry so as to examine the success of the surgery.
Methods: Records of patients who underwent nucleoplasty from two different university hospitals in Turkey were assessed. Records between 2005 and 2014 years of thirty-six cases, who had no recovery from medical and physical treatment and treated with nucleoplasty at single or double levels investigated retrospectively. All assessments included visual analog scale (VAS) evaluation before the surgery and at 6, 12, 24 and 36 months after the surgery. Intervertebral disc volumes between 4th and 5th cervical vertebrates and also between 5th and 6th were measured on axial magnetic resonance images slices using a stereological method, before and after the treatment.
Results: VAS results displayed pain improvement at 6, 12, 24 and 36 months after the surgery when compared with that of before the surgery (ps<0.05). After the nucleoplasty treatment, the mean intervertebral disc volumes between 4th and 5th, and also between 5th and 6th cervical vertebrates revealed significant decrease when compared with that of preoperative assesment (ps<0.05). The present study does not compare the results of different techniques used in the disc protrusion management.
Conclusions: Good classified patients may have good prognosis with nucleoplasty. The method is minimally invasive, provides a safer surgical experience and has protective effects on intervertebral disc biomechanics.
Keywords
Cervical disc herniation; Nucleoplasty; Coagulation; Intervertebral disc volume; Visual analog scale; Morphometry
Introduction
Cervical pain is usually the result of a complex interplay of biochemical and biomechanical processes. Internal disc disruption and disc heniations are common causes of cervical and/or upper extremity pain which may become chronic if not diagnosed and treated on time. Annular tears lead to migration of the nuclear contents and derange internal architecture. In the chronically injuried intervertebral disc, leakage of nuclear contents from annular tears may initiate, induce, and continue the inflammatory episode and delay or stop improvement of vital remaining intradiscal tissue [1]. Matrix metalloproteinases, phospholipase A2, cyclooxygenase, prostaglandins, nitric oxide, cytokines and interleukins were stated as the prominent mediators. Infiltration of macrophages and other inflammatory cells may induce neovascularization in the outer area of the annulus fibrosus allowing infiltration by inflammatory cell groups bringing extra cellular inflammatory initiators. Sensitization of the central nevous system has also been suggested to be a possible causative factor of chronicity in some cervical pain conditions. Disc herniation has been defined as displacement of the nucleus pulposus. The most uniformly accepted terminologies have been firstly described by Singh and Derby [2] as disc protrusion or herniation in which annulus fibrosus bulges markedly but is not stil ruptured, thus allowing no connection between the nucleus and the extra discal space; secondly extrusion or incomplete bulging-the annulus is ruptured but any expelled nucleus is stil connect with the rest of the disc. Finally complete bulging-disc tissue is expelled from the disc and is no longer connection with it [2,3]. Increased pressure from a displaced matrix induces nociceptors in the outer annulus fibrosus. The posterolateral portion of disc is the most important structure during injury and herniations due to the arrangement of the disc lamellae. The severity of the symptoms does not always associate with the extent of the bulging. Herniated discs pressurize to neural structures and causing radicular pain and radiculopathy. Cases with small bulging or annular tears with generous axial limb pain are candidate for percutaneous decompression has been discussed. Smaller bulging are hypothesized to cause referred limb pain due to neural inflammation and axial pain due to a both sensitized outer annulus fibrosus and increased annular pressure [4]. Several studies have reported decrement in inflammatory cytokines in rabbits and in Petri dishes after laser heat vaporization to nucleus pulposus and bipolar radiofrequency heat ablation therapy [2,5]. The most often refered purpose of central nuclear decompression is to lower nuclear compression and to allow space for herniated fragment to be expansion inward. Using nuclear coblation, Chen et al. [6] showed a 100% drop in compression in normal disc in young cadavers, but a unessential drop in pressure in degenerated lumbar discs following making six channels within each disc by applying the ablation and coagulation with coblation technique. Traditional standard open cervical discectomy, together with or without bony fusion, neurosurgical knowledge is accepted as the standard procedure for cervical disc herniation. However, percutan nucleoplasty is accepted as a minimally invasive application for healing chronic discogenic cervical pain in cases failing traditional standard treatment. Percutaneous intradiscal nucleoplasty is recently progressed method combining tissue ablation and thermal coagulation techniques, so is called as ‘‘coblation method’’. This modality offered decreased morbidity, not needed bone graft and pledge shorter improvement time [7]. The purpose of this study is to evaluate the effect of cervical nucleoplasty in patients failing conservative treatment using visual analog scale pain assesmant and intervertebral disc volumes.
Methods
Clinical analysis
We retrospectively analyzed a case series of single or double level nucleoplasty cases who had no recovery from medical and physical treatment and underwent nucleoplasty. All data used for this multicentric study were collected from 2005 to 2014 after institutional ethical approval was obtained from the university (Number: 012205). According to archive records totally 36 patients underwent nucleoplasty procedure during the time interval. Twenty-five of these underwent the procedure at single level, and the other eleven underwent the nucleoplasty procedure at double levels. The sides of the nucleoplasty treatment were not taken into account. All the patients had follow-up period up to 36 months. According to the file records, the patients had neck and arm pain more than 3 months and did not response to any medical therapy that contained analgesic-antiinflamatory and myorelaxan drugs.
We had some inclusion criterias according to the surgeons’ assesments including radicular symptoms, contained disc, failed conservative treatment, disc height >50%, discography concordant and the exclusion criterias; spinal fracture and tumor, extruded disc, complete annular disruption, moderate to severe spinal stenosis. Nucleoplasty was performed to the cases with chronic pain symptom which were not response any medical teraphy. The cases had no additional neurodeficit. Because of these reasons, clinical control group could not be able to created to compare the results; only before coblation and after coblation magnetic resonance ımaging (MRI) results on intervertebral discs volumetry and visual analog scale (VAS) values were compared for each of the cases. VAS was evaluated by a 10 point numeric rating scale, ranging from no aggravated pain “0” to the worst aggravated pain “10”.
The procedure was performed under general anaesthesia using a standart lateral discogram technique using a Perc-DC SpineWand connected to a system 2000 generator (ArthroCare Corp., Sunnyvale, CA) and 19 gauge, 4" introducer needle with trocar tip. Catheter positions and locations were assessed by fluoroscopy. Assessments included both preoperative and postoperative VAS and also intervertebral disc volumes on MRI were obtained, retrospectively.
Stereological analysis
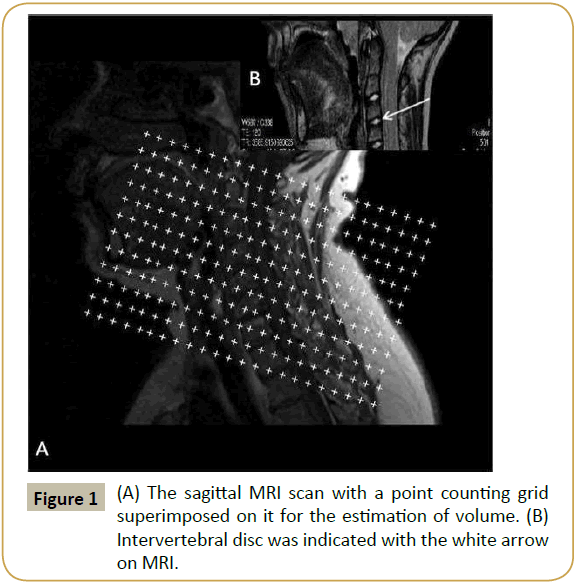
Intervertebral disc volumes which were between 4th and 5th (C4-C5) cervical vertebrates and also between 5th and 6th (C5- 6), were computed from MRI of 36 cases were measured three times by three observers using a stereological method. We measured 25 patients who had nucleoplasty at single level [C4- C5 (n=12) or C5-C6 (n=13)] patients, and 11 patients who had double level (C4-C5 and C5-C6) treatment. All measurements were performed by blinded researchers. An optimal plan was taken as the smallest diameter of anisotropic structures that can be measured in volumetric analysis of sagittal and coronal MRI sections. Original images were exported as “ .tiff” image files which were further subjected to stereological analysis. A uniform point-grid with a point-associated area of 0.625 cm2 was randomly superimposed on each image using the “Grid” (Figure 1). Points hitting the intervertebral disc were manually counted for volume estimation for each of the level. The volumes were also estimated using the Cavalieri’s principle of stereological methods as described previously [8,9]. Volume estimation was accomplished according to previously defined formula [8,10,11]:
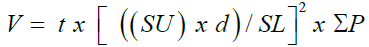
Where, t was the section thickness, SU was the scale unit (the real length of the scale marked on the MRIs), d was the distance between two points in the point grid, SL was the scale length (the actual measure of the scale on MRIs) and P was the number of points counted. All data had been entered into a previouslyprepared Microsoft excel spreadsheet for automatic calculation of the outcomes of the above formula and the statistical evaluation parameters including the nugget variance and the coefficient of error (CE).
Statistical analysis
Shapiro-Wilk’s and Levene’s test were used to assess the normality of distributions of the variables and the homogeneity of variances. Variables with normal distribution and homogeneous variance were analysed by Student’s t-test or paired samples t-test for comparisons of the two independent or dependent groups, respecvtively. Parametric test assumptions were not available for the statistical analysis of the VAS values, so the comparisons were performed with the Mann-Whitney U (males and females) test and with the Friedman test for dependent groups. The Friedman test was followed with the post-hoc analysis of Wilcoxon signed-rank test and Bonferroni correction. The results of tests were expressed as the number of observations (n), the mean ± standard deviation and the median (mean ± SD, M). Data analyses were performed with SPSS 15.0 software (statistical package for the social sciences, version 15.0, SSPS Inc, and Chicago IL, USA). A p value less than 0.05 was considered as statistically significant.
Results
We evaluated all the VAS values of the thirty six patients (16 males, 20 females) before and after the surgery without considering the sides and the levels of the disc herniations. The mean age of the patients was (mean ± SD) 42.00 ± 9.60 in males, 40.54 ± 9.49 in females and 41.11 ± 9.42 in all (males and females). The VAS values which were evaluated before and after the nucleoplasty were presented in Table 1. The VAS values were not statistical different between males and females at all evaluations before and after the nucleoplasty (p>0.05). Therefore, the VAS values were analysed in total (males and females). Pain perception of the six patients continued at mild level after the operation. The rest of the patients had good results about pain perception. The VAS values significantly improved at 6, 12, 24, 36 months after the treatment when compared to that of before the surgery (ps=0.000). There were no significant difference among the evaluations that were performed after the nucleoplasty (p>0.05).
| Measurement of VAS values | Males (n=16) (Mean ± SD; M) | Females (n=20) (Mean ± SD; M) | Total (n=36) (Mean ± SD; M) |
|---|---|---|---|
| Before nucleoplasty | 9.00 ± 0.87; 9 | 8.95 ± 0.78; 9 | 8.97 ± 0.81; 9 |
| After nucleoplasty | |||
| 6 months | 2.50 ± 1.50; 2.00 | 1.81 ± 1.00; 2.00 | 2.08 ± 1.25; 2.00 |
| 12 months | 2.35 ± 1.08; 2.00 | 1.81 ± 1.13; 2.00 | 2.02 ± 1.13; 2.00 |
| 24 months | 2.42 ± 1.08; 2.50 | 2.00 ± 1.27; 2.00 | 2.16 ± 1.20; 2.00 |
| 36 months | 2.57 ± 1.01; 3.00 | 2.04 ± 1.04; 2.00 | 2.25 ± 1.05; 2.00 |
| SD: Standard deviation, M: Median; N: Number of the observations, VAS: Visual analog scale. | |||
Table 1: Visual analog scale values of the patients before and after the nucleoplasty treatment.
Of the 36 patients, 25 patients had nucleoplasty at single level [C4- 5 (n=12; 5 males, 7 females) or C5-C6 (n=13; 6 males, 7 females)] patients, and 11 patients (5 males, 6 females) who had double level (C4-5 and C5-C6) treatment. Additionally, all the double level nucleoplasties were at the same side (right or left) and at the sequential levels. The intervertebral disc volumes were evaluated as concerning the nucleoplasty levels, so the intervertebral disc volumes were measured and analysed at C4-C5 and C5-C6 levels before and after the treatment. The intervertebral disc volumes before and after the surgery were presented in Table 2. There were no statistical significant difference between males and females, regarding the mean intervertebral disc volumes which were measured at C4-C5 and C5-C6 levels before and after the surgery (ps>0.05). Additionally, there were significant diferences between the intervertebral disc volumes at C4-C5 and C5-C6 levels which was obtained from the measurements before and after the surgery (ps=0.000 for both). The intervertebral disc volumes significantly reduced nearly 3.5% for females and 4% for males due to nucleoplasty treatment. The calculated CE values were given in Table 2.
| Intervertebral disc volumes (cm3) (Mean ± SD; M) | ||||
|---|---|---|---|---|
| C4-5 | C5-6 | |||
| Before | After | Before | After | |
| Males | 2.62 ± 0.34; 2.64, n=10 | 2.53 ± 0.35; 2.54 n=10 | 2.71 ± 0.35; 2.81 n=11 | 2.60 ± 0.35; 2.68 n= 11 |
| Females | 2.53 ± 0.43; 2.56, n=13 | 2.43 ± 0.46; 2.48 n=13 | 2.59 ± 0.39; 2.54 n=13 | 2.48 ± 0.38; 2.46 n= 13 |
| Total | 2.57 ± 0.39; 2.57 n=23 CE=0.050 | 2.47 ± 0.41; 2.48 n=23 CE=0.045 | 2.64 ± 0.37; 2.60 n=24 CE=0.042 | 2.53 ± 0.37; 2.48 n=24 CE=0.044 |
| SD: Standard deviation, M: Median; N: Number of the observations; CE: Coefficient error. | ||||
Table 2: Intervertebral disc volumes before and after the nucleoplasty treatment.
Discussion
Percutan cervical nucleoplasty is a minimally invasive technique for controlling chronic discogenic cervical pain [10-12]. Azzazi et al. described the inclussion criterias for planning nucleoaplastyas disc protrusion or contained herniated disc <6 mm with a disc height >50% of the adjacent disc heights [7,13,14]. Although there were many retrospective and prospective outcome studies for lumbar discs, but there were restricted studies published about the clinical outcomes of the cervical nucleoplasty cases including pain assesment and intervertebral disc volumes [13,15,16].
Percutaneous disc decompression with nucleoplasty (coblation technology) was performed with radio frequency (RF) energy to dissolve nuclear material through molecular dissociation. Bipolar RF coagulation denatured proteoglycans and led to reduction in intradiscal pressure of the nucleus pulposus by changing the internal structure [6,12,17]. The effectiveness of nucleoplasty was reported in several prospective evaluations [7,17-20]. There were no randomized trials regarding the effectiveness of percutaneous disc decompression with nucleoplasty. However, all the observational studies showed significant improvements in short-term, as well as long term, in numerous parameters with pain and functional status. All the investigations were designed in cases either with disc induced pain or with small contained disc protrusions. In literature, there were no studies to compare the clinical results of percutaneous nucleoplasty and percutaneous cervical discectomy related with cervical disc herniation [21]. Castro et al. [22] showed that, the disc space narrowed approximately 1.42 mm and the disc protrusion increased 0.45 mm for per gram of removed nucleus pulposus. 4 g to 5 g of nucleus pulposus was remowed during open discectomy operation. Whereas, 1 g of nucleus pulposus was vaporized during nucleoplasty procedure. If the outcome was similar, the preferable method was nucleoplasty technique due to long term stability and remowing less amounts. During nucleoplasty the aim was vaporazing the center of the nucleus pulposus for allowing room for the protrused component of implode inward. Nucleoplasty carries a small number of complications. Some complications include; infections, bleeding, nerve damage, worsened pain, failure of technique, recurrent herniation, paralysis, catheter fracture. According to the file records, one patient had catheter breakage at intradiscal space, so the patient underwent open discectomy, and she was excluded from the study. Although pain of the six patients continued at mild level after nucleoplasty, the postoperative VAS values of the other patients were significantly decreased.
Preoparative and postoperative intervertebral disc volumes were also evaluated. We recorded significant differences at C4-C5 and C5-C6 levels on the intervertebral disc volumetry between the cervical nucleoplasty cases for both sexes with using coblation technique. In literature, there were limited data on intervertebral disc height evaluation, there was no results on the volumetrical analysis of the discs. Although intervertebral disc volumes of the patients decreased after nucteoplasty, there were no biomechanical and anatomical changes. Pain percepsions of the patients were also diminished after the technique. Further studies will be designed on this method so as to compare between the coblation technique and the other methods such as conventional or the newest techniques such as laser discectomy or hydrodissection of discs etc.
Conclusion
According to our results, if patients are selected well, the outcomes and the patients’ satisfaction will be better. Surgeons should use inclusion criterias which mentioned above for a succesfull cervical nucleoplasty procedure. The techique is safe and effective in protecting the normal intervertebral disc biomechanics and anatomy.
References
- Miller MR, Mathews RS, Reeves KD (2006) Treatment of painful advanced internal lumbar disc derangement with intradiscal injection of hypertonic dextrose. Pain Physician 9: 115-121.
- Singh V, Derby R (2006) Percutaneous lumbar disc decompression. Pain Physician 9: 9-146.
- Ohnmess DD, Vanharanta H, Ekholm J (1997) Degree of disc disruption and lower extremity pain. Spine 22: 1600-1605.
- O’Neill CW, Kurgansky ME, Derby R, Ryan DP (2002) Disc stimulationand patterns of referred pain. Spine 27: 2776-2781.
- Iwatsuki K, Yoshimine T, Sasaki M, Yasuda K, Akiyama C, et al. (2005) The effect of laser irradiation for nucleus pulposus: an experimental study. Neurol Res 27: 319-323.
- Chen YC, Lee SH, Chen D (2003) Intradiscal pressure study of percutaneous disc decompression with nucleoplasty in human cadavers. Spine 28: 661-665.
- Nardi PV, Cabezas D, Cesaroni A (2005) Percutaneous cervical nucleoplasty using coblation technology. Clinical results in fifty consecutive cases. Acta Neurochir Suppl 92: 73-78.
- Acer N, Sahin B, Usanmaz M, Tatolu H, Irmak Z (2008) Comparison of point counting and planimetry methods for the assessment of cerebellar volume in human using magnetic resonance imaging: A stereological study. Surg Radiol Anat 30: 335-339.
- Gocmen-Mas N, Pelin C, Canan S, Yazici AC, Zagyapan R, et al. (2009) Stereological evaluation of volumetric asymmetry in healthy human cerebellum. Surg Radio Anat 31:177-181.
- Ekinci N, Acer N, Akkaya A, Sankur S, Kabadayi T, et al. (2008) Volumetric evaluation of the relations among the cerebrum, cerebellum and brainstem in young subjects: a combination of stereology and magnetic resonance imaging. Surg Radiol Anat 30: 489-494.
- Kalkan E, Cander B, Gul M, Girisgin S, Karabagli H, et al. (2007) Prediction of prognosis in patients with epidural hematoma by a new stereological method. Tohoku J Exp Med 211: 235-242.
- Boswell MV, Trescot AM, Datta S, Schultz DM, Hansen HC, et al. (2007) American Society of Interventional Pain Physicians. Interventional techniques: evidence-based practice guidelines in the management of chronic spinal pain. Pain Physician 10: 70-111.
- Cesaroni A, Nardi PV (2010) Plasma disc decompression for contained cervical disc herniation: a randomized, controlled trial. Eur Spine J 19: 477-486.
- Azzazi A, Al Mekawi S, Zein M (2011) Lumbar disc nucleoplasty using coblation technology: Clinical outcome. J Neurointerv Surg 3: 288-292.
- Kim SH, Kim SC, Cho KH (2012) Clinical outcomes of percutaneous plasma disc coagulation therapy for lumbar herniated disc disease. J Korean Neurosurg Soc 51: 8-13.
- Li J, Yan DL, Gao LB, Tan PX, Zhang ZH, et al. (2006) Comparison percutaneous cervical disc nucleoplasty and cervical discectomy for the treatment of cervical disc herniation. Zhonghua Wai Ke Za Zhi 44: 822-825.
- Chen YC, Lee SH, Saenz Y, Lehman NL (2003) Histologic findings of disc, end plate and neural elements after coblation of nucleus pulposus: an experimental nucleoplasty study. Spine J 3: 466-470.
- Sharps LS, Isaac Z (2002) Percutaneous disc decompression using nucleoplasty. Pain Physician 5: 121-126.
- Singh V, Piryani C, Liao K, Nieschultz S (2002) Percutaneous disc decompression using coblation (nucleoplasty) in the treatment of chronic discogenic pain. Pain Physician 5: 250-259.
- Singh V, Piryani C, Liao K (2004) Role of percutaneous disc decompression using coblation in managing chronic discogenic low back pain: a prospective, observational study. Pain Physician 7: 419-425.
- Yan D, Li J, Zhu H, Zhang Z, Duan L (2010) Percutaneous cervical nucleoplasty and percutaneous cervical discectomy treatments of the contained cervical disc herniation. Arch Orthop Trauma Surg 130: 1371-1376.
- Castro WH, Halm H, Rondhuis J (1992) The influence of automated percutaneous lumbar discectomy (APLD) on the biomechanics of the lumbar intervertebral disc. An experimental study. Acta Orthop Belg 58: 400-405.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences