Microsurgical Anterior Cervical Foraminotomy (Uncoforaminotomy) for the Treatment of Compressive Radiculopathy
Marcos Baabor, Fabian Piedimonte, Cristobal Vergara, Consuelo Guzman and Pablo Baabor
DOI10.21767/2471-8173.100031
Marcos Baabor1*, Fabian Piedimonte2, Cristobal Vergara1, Consuelo Guzman1 and Pablo Baabor3
1Department of Neurology and Neurosurgery, University of Chile, Medical School, Chile
2Fundacion CENIT, Buenos Aires, Argentina
3University San Sebastian, Santiago, Chile
- *Corresponding Author:
- Marcos Baabor
Department of Neurology and Neurosurgery
University of Chile, Medical School, Chile
Tel: +562 29788260
E-mail: marcosbaabor@yahoo.com
Received Date: January 09, 2017 Accepted Date: July 15, 2017 Published Date: July 19, 2017
Citation: Baabor M, Piedimonte F, Vergara C, Guzman C, Baabor P (2017) Microsurgical Anterior Cervical Foraminotomy (Uncoforaminotomy) for the Treatment of Compressive Radiculopathy. Spine Res. Vol. 3 No. 2:11 doi:10.21767/2471-8173.100031
Abstract
Cervical radiculopathy is typically caused because of posterolateral disc herniation or spondylotic foraminal stenosis. Most of the times, either direct anterior excision necessitating fusion or indirect posterior decompression is used as a standard surgical treatment for the same. However, anterior decompression has been used widely. Different techniques can be used. The authors report the clinical application of a new microsurgical technique. The cervical anterior foraminotomy (uncoforaminotomy), which is used for the surgical treatment of unilateral cervical radiculopathy secondary to posterolateral disc herniations or spondylotic foraminal stenoses.
https://transplanthair.istanbul
https://hairclinicturkey.co
https://hairclinicistanbul.co
https://besthairtransplant.co
https://hairtransplantistanbul.co
Keywords
Anterior cervical foraminotomy; Disc herniation; Spondylotic foraminal stenosis; Nerve root decompression
Introduction
Compressive cervical radiculopathy is commonly caused by disc or spondylotic pathology, and both can be treated surgically by anterior or posterior access. Usually choosing one or another approach depends on the pathology as well as the surgeon´s own preference.
The first report on cervical herniated disc successfully treated by laminectomy was published in 1934 by Mixter and Barr [1]. In 1944, Sperling and Scoville [2] reported cervical disc removal using laminectomy in a large series. Form that moment on, the posterior access for treating cervical radiculopathy evolved to minimal lateral foraminotomy, also known as keyhole, popularized by Frykholm [3]. Although posterior cervical keyhole maintains function on the affected side, it only achieves indirect decompression of the nerve root, and does not allow direct removal of an eventual ventromedial lesion that may compress the nerve root, with the exception of soft disc fragments [4-9]. Posterior access limitations led to the development of the anterior access to the cervical spine, and to anterior cervical discectomy with and without intervertebral fusion in the 1950´s by Cloward [10] and Smith and Robinson [11], and has been adopted by many authors since then [12-20]. However, anterior intervertebral fusion and anterior cervical diskectomy without fusion, which culminates in spontaneous arthrodesis as well as part of its natural evolution, result in loss of mobility and function of the compromised vertebral segment [16-21].
The objective of avoiding the morbidity associated to vertebral fusion, including those complications related to the graft itself, graft´s donor site and the disease of the adjacent cervical level on one side, and considering the advances in radiology [22-24] that allow a thorough, detailed and precise evaluation on the other side, led to the development of minimally invasive surgical techniques through anterior access. These intended to treat anterior compressive foraminal lesions which do not require, unlike classical techniques, the complete disc removal nor the implant of intersomatic prosthetic devices, achieving direct and complete decompression of the root while maintaining the intervertebral disc in its shape and function, preserving both stability and mobility of the affected segment.
Surgical Technique
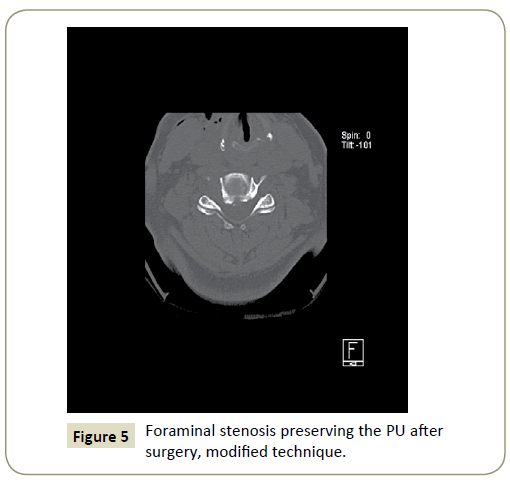
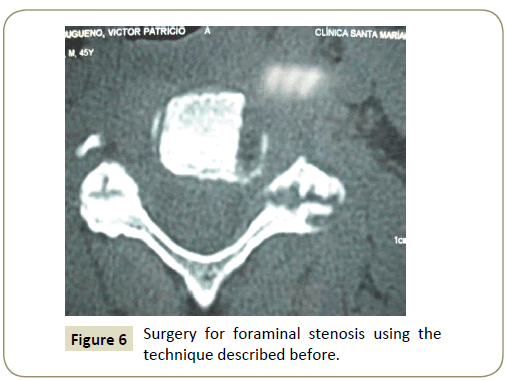
In this paper we propose and describe a minimally invasive technique for microsurgical anterior cervical decompression of the foramen, which is based on the technique described by Jho [25], but modified to preserve the majority of the processus uncinatus, maintaining a better stability upon the cervical segment.
The surgical approach has previously been reported and does not differ significantly from the approach required for conventional anterior cervical diskectomy [11-21]. The patient was given general anesthesia and placed in supine position on the operating table with the head in neutral position. The cervical spine was slightly extended to increase the lordosis using a gel cushion under the shoulders. It was not necessary the use of cervical traction devices nor caudal fixation of the upper limbs. The shoulders were attached to the surgical table with adhesive tape to improve the fluoroscopic vision. The approach was done ipsilateral to the radiculopathy. The correct vertebral level and site of skin incision was identified using preoperatively fluoroscopic guidance with X-rays and a needle lateral to the neck. Subsequently, sterile operative field was set placing surgical drapes.
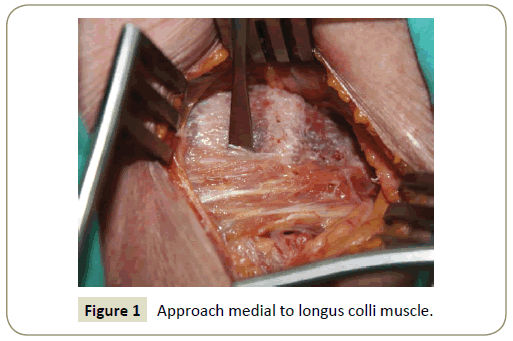
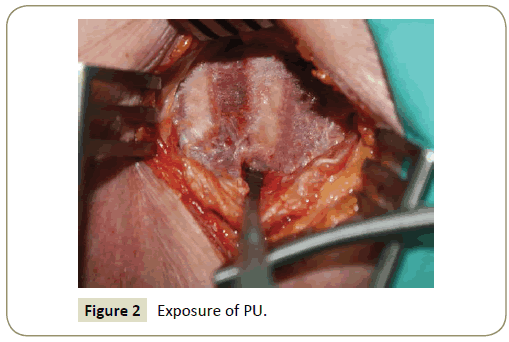
Transversal skin incision of 3 cm to 4 cm was made in the confirmed cervical level, two-thirds medially and one-third laterally to the anterior border of the sternocleidomastoid muscle. The platysma was dissected along the skin incision. The access to the cervical spine was achieved through blunt dissection starting from the opening of the superficial fascia at the anterior border of the sternocleidomastoid muscle, maintaining the visceral structures medially and the neurovascular bundle laterally. The prevertebral fascia was opened exposing the anterior aspect of the vertebral bodies, the intervertebral disc and the medial portion of the longus colli muscle. The correct level was again confirmed by X-rays in lateral view. Under microscopic view, the longus colli wass disinserted subperiostically (Figure 1) and then reflected laterally, covering a length of 12 mm to 16 mm, and thus exposing approximately 6 mm caudally and 10 mm rostrally to the inferior margin of the disc space in question. This way, visualization of the whole processus uncinatus was achieved (Figure 2). At the level of C7 extreme care must be taken to avoid injury to the vertebral artery, which runs between the transverse process and the longus colli. Unlike Jho’s technique, the vertebral artery was not exposed deliberately in this approach [25].
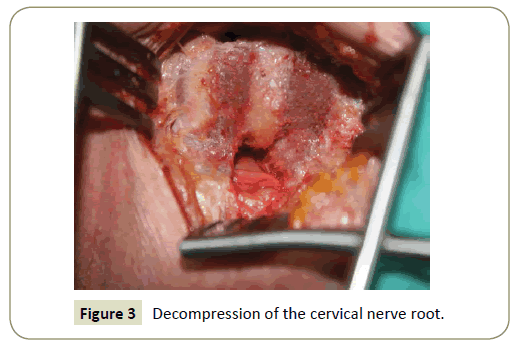
At this stage, under microscopic view, the surgical field was limited cranially, caudally and laterally by the longus colli. This muscle, reflected laterally, acted as an additional protective plane to the vertebral artery. The exposed field involves the lateral third of the intervertebral disc, the lateral portion of the inferior vertebral body including the corresponding processus uncinatus (PU) and the lateral aspect of the superior vertebral body. Using a high-speed drill and a 1.8 mm spherical bur, proceeded to cut the external side of the PU, conforming a semi-oval orifice of 2 mm to 3 mm wide and 8 mm to 10 mm high. Drilling was performed, reaching the posterior cortical laminae or directly to the dura of the corresponding nerve root. Using a 2 mm spherical diamond bur we proceeded to resect the thinned posterior cortical layer and the posterior part of the lateral wall of the PU carefully drilling it. Through this procedure, posterolateral osteophytes as well as the external and foraminal part of the PU were removed, and so the underlying root was decompressed under microscopic view (Figure 3). In some cases, a thin cortical bone layer of the lateral wall of the PU can be maintained in order to keep a landmark and as a protection for the subjacent vertebral artery. In such cases, the periosteum covered the nerve root, disc fragments and the lateral aspect of the posterior longitudinal ligament (PLL). When the bone covert was not maintained, the safety limit was provided by the venous plexus surrounding the vertebral artery.
Periosteum, fibrous cartilage tissue and degenerative tissue found between the apex of the PU and the inferior plate of the upper vertebral body were removed with a 1 mm or 2 mm Kerrison rongeur. Osseus decompression of the nerve root caused by bone anomalies such as osteophytes or posterolateral bone spurs in the inferior terminal plate of the inferior vertebral body were removed using the same Kerrison rongeur. The maneuver was performed at the foramen, from lateral to medial.
Fragments of the herniated disc could be identified in front of the underlying nerve root. Such fragments were safely removed from the disc using microsurgical hooks and clamps.
At this stage, the lateral aspect of the PLL covered the lateral part of the dural sac and the origin of the nerve root. Posterior Longitudinal Ligament was then elevated with a microsurgical hook, and if a sequestered disc was found under the ligament, it could be resected with a 2 mm Kerrison Rongeur.
After all these steps, the complete nerve root was appreciated, from its origin to the intervertebral foramen, which could be approached without risks with a microsurgical hook inferiorly and superiorly to the nerve root, confirming it was entirely decompressed.
Finally, the skin retractor was removed, hemostasis was controlled meticulously, the platysma was sutured with separated reabsorbable stitches, and finally a hidden intradermal suture, without requiring drain devices. We did not use external fixation of the neck with a cervical collar.
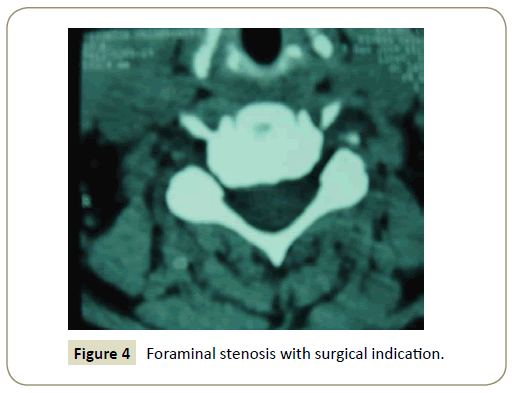
Patient could be dismissed at 24 hours after the surgery, and could return to work immediately, without the need for rehabilitation. We prescribed anti-inflammatory and/or analgesic pills for 2 days to 3 days. Medical control was appointed at 10 days after surgery (Figures 4-6).
Clinical Cases
Between January 2002 and December 2009, thirty-seven consecutive patients were surgically operated due to compressive cervical radiculopathy, using the surgical technique described above.
Patients were indicated surgery based on the following criteria:
1. Unilateral cervical radiculopathy refractory to medical therapy after 6 weeks of optimal treatment.
2. Absence of symptoms and signs of cervical myelopathy.
3. Compatible Imaging studies showing foraminal stenosis produced by osteophytes and/or a foraminal herniated disc, without spinal cord compression.
Fifteen of the patients were male and twenty-two were female, with an average age of 53 by the time of the surgical intervention (range 42 years to 68 years old). The duration of symptoms before surgery was 2 months to 26 months (average 7.8 months). (Table 1)
| Duration of symptoms | Number of patients |
|---|---|
| < 2 months | 2 |
| 2 months to 4 months | 10 |
| 4 months to 6 months | 12 |
| 6 months to 8 months | 6 |
| >12 months | 7 |
Table 1: Duration of symptoms before surgery in 37 patients.
All patients were studied with radiographic dynamic imaging of the cervical spine in lateral view (maximum extension, maximum flexion and neutral). In addition, all 37 patients had cervical spine MRI and CT scans to determine the relation and compromise of the nerve root and foramen.
Neurophysiological studies were not routinely made and was a part of the workup in those patients whose symptoms and imaging studies were not completely compatible.
Patients with bilateral symptoms and significant stenosis of the spinal canal, associated to myelopathy or severe alignment of the spine axis were not indicated with surgical intervention.
Results
All 37 patients had immediate radicular and cervical pain relief after surgery, with preservation of the normal range of movement of the neck and without morbidity related to surgery. Four out of nine patients with pre-operative paresis recovered the motor deficit within the first week after surgery. Those 5 patients who did not recover the motor function immediately continued physical rehabilitation until complete regain of strength the next 6 months after surgery in three patients, and 2 patients had a persistent mild motor deficit.
Sensory disturbance phenomena such as hypoaestesia, disestesy, etc improved immediately in 10 of 16 patients presenting with such findings. Depending on symptoms duration, sensory deficit improved gradually in the majority of the remaining 6 patients in weeks to months. The follow up time was from 2 months to 72 months, with an average of 32.6 months. During this time, no recurrence of radiculopathy was observed (Table 2).
| Follow up time | Number of patients |
|---|---|
| 2-11 months | 7 |
| 12-23 months | 6 |
| 24-35 months | 10 |
| 36-47 months | 6 |
| 48-60 months | 5 |
| 60-72 months | 3 |
Table 2: Follow Up time of 37 patients.
Since all patients had notorious clinical improvement without recurrence of radicular pain, we did not perform routine MRI nor CT scans during the follow up time.
Discussion
Development and dissemination of the anterior cervical approach, initially proposed by Smith and Robinson and then by Cloward, may be considered the beginning of the age of anterior cervical diskectomy with and without fusion for the patients afflicted with cervical spondylotic radiculopathy [10,26]. This technique argued in favor of direct anterior decompression of the structures causing the symptoms, but had to face the many disadvantages inherent to the lowering of the disc´s height– in those cases of diskectomy without fusion– and the fusion a mobile cervical segment with consequent loss of function [16,27,28]. One of the main complications associated to the loss of mobility of a particular cervical segment is the adjacent segment´s appearance of the disease, with a reported incidence of 25% to 81% in different studies with long term follow-up [14,29,30]. The cause of the Adjacent´s Segment Syndrome, which is not fully elucidated, seems to be related to the increase in mechanical stress which leads to increased pressure of the disc at the contiguous level, resulting in osmotic gradients and metabolic disorder [31-33].Moreover, the anterior fusion technique has been related to a higher incidence of pseudoarthrosis and problems related to the bone graft [15,34,35].
Furthermore, the approach and indirect decompression through posterior foraminotomy has also been used to cervical radiculopathy, even when the lesion is located anteriorly to the nerve root and is not directly reached with this surgical procedure [36-38]. This approach is more suitable for the cervical radiculopathy secondary to a lateral herniated disc, localized lateral hypertrophy of the ligamentum flavum or facet joint arthropathy with secondary hypertrophic facet [36,39]. Lamino-foraminotomy is also associated to technical limitations conditioned by the restricted surgical view of the distal foramen, and an increased epidural bleeding [40]. Additionally, this technique has a higher incidence of postoperative muscle contracture, neck pain and a longer recovery period, probably due to the muscular dissection needed to expose the surgical site [39]. Although several long term studies have reported successful outcomes using the lamino-foraminotomy technique, this is not the optimal treatment for most of the patients suffering cervical radiculopathy who usually present a mixed disease of herniated disc and spondylotic osteophytes located anteriorly to the nerve root.
Therefore, an anterior approach that does not affect the segmental mobility and that offers at the same time the opportunity to resolve the pathologic lesion responsible for the compression becomes the natural choice in the evolution of the treatment of cervical radiculopathy. This enhances the concept known as “functional cervical surgery”, term coined by Jho [36]. Snyder and Bernhardt were the first surgeons attempting a technique without fusion maintaining the disc for the anterior foraminal decompression, but this technique still required the removal of the lateral third of the intervertebral disc [11]. George et al. [41] resumed the original technique reported by Verbiest of oblique transcorporal approach for the lesions located anteriorly in the cervical spinal canal, exposing the vertebral artery with the associated risks of the procedure.
In 1996 Jho [25] was the first to describe the anterior transnuchal foraminotomy, emphasizing the preservation of the disc space. However, this technique still demanded the exposure of the vertebral artery along it´s medial surface. Saringer in the year 200, proposed a modified trans nuchal technique preserving a thin layer of cortical bone of the lateral aspect of the PU, avoiding the exposure of the vertebral artery [42]. Anyhow, the transversal dissection of the sternocleidomastoid muscle of at least 10 mm was needed, thus favoring the injury of the cervical sympathetic chain expressed as Horner´s Syndrome. Because both techniques mentioned above use a relatively low transcorporal vertebral approach, situating the opening caudally to the compressive lesion due to the obliquity of the vertebral disc, and thus requiring a larger osseous and soft tissue resection to achieve adequate decompression. In the year 2002, Jho [36], based on his previous experience, reported a vertebral transcorporal foraminotomy technique locating the opening of the foraminotomy rostrally, overcoming to some of the disadvantages of the lower vertebral transcorporal approach. Using this technique, Jho claimed that the surgical target was approached easily and preserving the intervertebral disc.
Of all the different techniques, the one described by us is the only one that does not require to expose the vertebral artery, diminishing the risk of arterial injury. Locating the foramen medially to the sternocleidomastoid muscle helps in avoiding Horner´s Syndrome, using this muscle as a protection of the vertebral artery and the sympathetic chain, facilitating even more this technique. By preserving most of the PU, the stability of the segment is not compromised if partial diskectomy is needed to access the conflicted region.
A potential problem with this technique is the risk of vertebral collapse during the early postoperative period, because the foraminotomy opening acts as a mechanical stressing factor. With our technique, this problem is minimized since most of the vertebral body remains mostly unscathed (untouched). Anyhow, this risk is rather theoretical than real, because the opening is only 12% of the vertebral area, and such complication has not been observed by any other research group.
Although the outcomes in these series are based in a small group of patients, the excellent results in the short and long term are encouraging. The absence of complications as the Horner´s Syndrome, recurrent laryngeal nerve palsy, the minimization of injuries to the vertebral artery, together with the maintenance in the stability of the cervical segment, proof of the benefits of this technique. A strict patient-inclusion criteria, and a direct access to the compressive lesions are some of the contributing factors to an optimal outcome in most of the patients operated with this technique.
Conclusion
Anterior cervical microforaminotomy is a minimally invasive procedure, simple to perform, highly effective in the short and long term to treat the foraminal compressive cervical radiculopathy. Preservation of most of the disc, associated to minimal aggression on the bone structures ensure the functional maintenance of the affected segment, which is reflected in a rapid and complete recovery in those patients treated, allowing immediate and total social and labor reintegration.
The need of a surgical microscope and high-speed drill as the only condition required to perform this procedure turns it into a costeffective technique, unfortunately underused, but with a high potential to be promoted in our region.
The main difference of the proposed technique compared to the previous one is that it is much more anatomic and minimally invasive, with the preservation of at least 70 or more percent of the PU, as shown in cadaveric specimens step by step.
References
- Miter WJ, Barr JS (1934) Rupture of the intervertebral disc with involvement of the spinal canal. N Engle J Med 211: 210-215.
- Spelling RG, Sackville WB (1944) Lateral rupture of the cervical intervertebral disc. A common cause of shoulder and arm pain. Surg Gynecol Obstet 798: 350-358.
- Frykholm R (1951) Root compression resulting from disc degeneration and root sleeve fibrosis. Acta Chi Scand 160: 1-149.
- Adamson TE (2001) Microedoscopic posterior cervical laminoforaminotomy for unilateral radiculopathy: Results of a new technique in 100 cases. J Neurosurg Spine 95: 51-57.
- Aldrich F (1990) Posterolateral microdiscectomy for cervical monoradiculopathy caused by posterolateral soft cervical disc sequestration. J Neurosurg 72: 370-377.
- Krupp W, Schattke H, Muke R (1990) Clinical results of the foraminotomy as described by Frykholm for the treatment of lateral cervical disc herniation. Acta Neurochir 107: 22-29.
- Mosdal C, Overgaard J (1984) Lateral cervical facetectomy. The surgical pathology of radicular brachialgia. Acta Neurochir 70: 199-205.
- Simeone F, Dillin W (1986) Treatment of cervical disc disease: Selection of cervical approach. Contemp Neurosurg 8: 16.
- Williams RW (1983) Microcervical foraminotomy. A surgical alternative to intractable radicular pain. Spine 8: 708-716.
- Cloward RB (1958) The anterior approach for removal of ruptured cervical discs. J Neurosurg 15: 602-614.
- Smith GW, Robinson RA (1958) The treatment of certain cervical spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg (Am) 42: 607-623.
- Bertalanffy H, Eggert HR (1988) Clinical long-term results of anterior discectomy without fusion for treatment of cervical radiculopathy and myelopathy. A follow-up of 164 cases. Acta Neurochir 90: 127-135.
- Clements DH, O’Leary PF (1990) Anterior cervical discectomy and fusion. Spine 15: 1023-1025.
- DePalma AF, Rothman RH, Lewinnek GE (1972) Anterior interbody fusion for severe disc degeneration. Surg Gynecol Obstet 134: 755-758.
- Lundsford LD, Bissonette JD, Jannetta PJ (1973) Anterior surgery for cervical disc disease. Part 1: Treatment of lateral cervical disc herniation in 253 cases. J Neurosurg 53: 679-683.
- Martins AN, Albert N, Colonel M (1976) Anterior cervical discectomy with and without interbody bone graft. J Neurosurg 44: 290-295.
- Matge G (1998) Anterior interbody fusion with the BAK-cage in cervical spondylosis. Acta Neurochir 140: 1-8.
- Murphy MG, Gado M (1972) Anterior cervical discectomy without interbody bone graft. J Neurosurg 37: 71-74.
- Savoluinen S, Usenius JP, Hernesniemi J (1994) Iliac crest versus artificial bone grafts in 250 cervical fusions. Acta Neurochir 129: 54-57.
- Watters WC, Levinthal R (1983) Anterior cervical discectomy with and without fusion. Results, complications, and long-term follow-up. Spine 19: 708-716.
- Hakuba A (1976) Trans-unco-discal approach. A combined anterior and lateral approach to cervical discs. J Neurosurg 45: 284-291.
- Hedberg MC, Drayer BP, Flom RA (1988) Gradient echo (GRASS) MR imaging in cervical radiculopathy. AJR 150: 683-689.
- Miyasaka K, Isu T, Iwasaki Y (1983) High resolution computed tomography in the diagnosis of cervical disc disease. Neuroradiology 24: 253-257.
- Modic MT, Weinstein MA, Pavlicek W (1983) Magnetic resonance imaging in the cervical spine: Technical and clinical observations. AJR 141: 1129-1136.
- Jho HD (1996) Microsurgical anterior cervical foraminotomy for radiculopathy: A new approach to cervical disc herniation. J Neurosurg 84: 155-160.
- Schimandle JH, Boden (2003) Degenerative disorders of the cervical spine: cervical radiculopathy. In: Emery SE, Boden SD (eds) Surgery of the cervical spine, Saunders. Elsevier Science, Philadelphia, USA. p. 94.
- Hankinson HL, Wilson CB (1973) Use of the operating microscope in anterior cervical discectomy without fusion. J Neurosurg 43: 452-456.
- Urban JP, Holm S, Maroudas A (1982) Nutrition of the intervertebral disc: Effect of fluid flow on solute transport. Clin Orthop Relat Res 296-302.
- Dmitriev AE, Cunningham BW, Hu N (2005) Adjacent level intradiscal pressure and segmental kinematics following a cervical total disc arthroplasty: An in vitro human cadaveric model. Spine 30: 1165-1172.
- Hilibrand AS, Yoo JU, Carlson GD (1997) The success of anterior cervical arthrodesis adjacent to previous fusion. Spine 22: 1574-1579.
- Pospiech J, Stolke D, Wilke HJ (1999) Intradiscal pressure recordings in the cervical spine. Neurosurgery 44:379-385.
- Snyder GM, Bernhardt AM (1989) Anterior cervical fractional interspace decompression for treatment of cervical radiculopathy. A review of the first 66 cases. Clin Orthop 246: 92-99.
- Urban JP, Holm S, Maroudas A (1977) Nutrition of the intervertebral disk. An in vivo study of solute transport. Clin Orthop Relat Res 101-114.
- Clements DH, O’Leary PF (1990) Anterior cervical discectomy and fusion. Spine 15:1023–1025.
- Saringer W, Nobauer I, Reddy M (2002) Microsurgical anterior cervical foraminotomy (Uncoforaminotomy) for unilateral radiculopathy: Clinical results of a new technique. Acta Neurochir 144:685–694.
- Jho HD, Kim WK, Kim MH (2002) Anterior microforaminotomy for treatment of cervical radiculopathy: Part i-disc preserving “functional cervical disc surgery”. Neurosurgery 51: 46-53.
- Raynor RB, Pugh J, Shapiro I (1985) Cervical facetectomy and the effect on spine strength. J Neurosurg 63: 278-282.
- Verbiest H (1968) A lateral approach to cervical spine: technique and indications. J Neurosurg 28: 191–203
- Fessler RG, Khoo LR (2002) Minimally invasive cervical microendoscopic foraminotomy: An initial clinical experience. Neurosurgery 51: 37-45.
- Ebersold MJ, Raynor RB, Bovis GK (1999) Cervical laminotomy, laminectomy, laminoplasty and foraminotomy. In: Benzel EC (ed) Spine surgery: Techniques, complication avoidance and management. Churchill Livingstone 251–253.
- George B, Zerah M, Lot G (1993) Oblique transcorporeal approach to anteriorly located lesions in the cervical spinal canal. Acta Neurochir 121: 187–190.
- Sampath P, Bendebba M, Davis J (1999) Outcome in patients with cervical radiculopathy: Prospective, multicenter study with independent clinical review. Spine 24: 591–597.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences