Is the Interspinous Device (Coflex) Outdated in the Treatment of Lumbar Spinal Stenosis? A Seven-Year Follow-up
Yin Dong, Zheng X, Gu H, Liang G, Zhuang J, Liang CX, Liu B and Chang Y
DOI10.21767/2471-8173.100042
Yin Dong*, Zheng X, Gu H, Liang G, Zhuang J, Liang CX, Liu B and Chang Y
Department of Orthopaedics, Guangdong General Hospital, Guangdong Academy of Medical Sciences, Guangzhou, P.R China
- *Corresponding Author:
- Dong Yin
Department of Orthopaedics, Guangdong General Hospital, Guangdong Academy of Medical Sciences
No. 106 Zhongshan Er Road, Yuexiu District, Guangzhou, P.R China.
Tel: +86-13189096848
Fax: +86 20 83827712
E-mail: tony-inn@163.com
Received Date: January 01, 2018; Accepted Date: January 25, 2018; Published Date: January 31, 2018
Citation: Dong Y, Zheng X, Gu H, Liang G, Zhuang J, et al. (2018) Is the Interspinous Device (Coflex) Outdated in the Treatment of Lumbar Spinal Stenosis? A Seven-Year Follow-up. Spine Res. Vol.4 No.1:2 DOI: 10.21767/2471-8173.100042
Abstract
Background: Coflex, a kind of dynamic interspinous spacer, has been widely used for the treatment of lumbar spinal stenosis in the past a few years. However, controversy remains as to whether dynamic interspinous spacer use is superior to traditional decompression and fusion surgery. High complication, reoperation rate, and costs with poor outcomes were also mentioned in the literature. The aim of the present study is to evaluate whether Coflex implantation following spinal decompression provided better clinical outcomes compared with traditional decompression and fusion for symptomatic lumbar spinal stenosis through midterm follow-up.
Methods and findings: A total of 100 patients who were confirmed L4/5 lumbar spinal stenosis was surveyed from June 2007 to June 2010. They were randomly and equally divided into two groups: 50 cases underwent spinal decompression with Coflex implantation, and 50 cases were treated with spinal decompression with fixation and fusion. The operation time, intraoperative blood loss, ambulation time, and hospitalization days, Japanese Orthopedic Association scores, visual analogue scale scores, Oswestry disability index and SF-36 scores were compared between the two groups. The ranges of motion and the height loss at adjacent segments (L3/4 and L5/S1) were measured preoperative and postoperative, respectively. Adjacent segment degeneration at L3/4 and L5/Sl was assessed by Pfirrmann classification. Complications were also recorded. The average age was 57.6 ± 5.9 years old in Coflex implantation group and 59.0 ± 6.7 years old in fusion group, respectively. The average follow-up period was 7.12 ± 1.1 year in Coflex implantation group and 7.31 ± 1.6 year in fusion group, respectively. JOA, ODI, VAS and SF-36 scores were improved at the last follow-up in all the two groups with significant differences (P<0.01) compared with those preoperative, but no statistical differences between the two groups (P>0.05). The intervertebral heights of adjacent segments were decreased at the last follow-up and the ranges of intervertebral motions were increased in both groups. The height loss and the range of motion increase of adjacent segments were greater in fusion group than those in Coflex group with statistical significant difference (P<0.01). At the last follow-up, adjacent segment disc Pfirrmann grade progressed more obviously in fusion group compared with that in Coflex group, and there was significant difference (P<0.05) between the two groups.
Conclusion: Based on the present study, it showed that Coflex implantation and fusion after spinal decompression had the same clinical outcomes and satisfaction in treatment of symptomatic lumbar spinal stenosis after 7 years follow-up. Nevertheless, Coflex implantation had the advantages of less bleeding loss, less trauma and quick recovery. Compared with fusion surgery, Coflex implantation had also advantages in maintaining intervertebral height and delaying intervertebral disc degeneration of adjacent segments.
Keywords
Coflex; Lumbar spinal stenosis; Fusion; Intervertebral height; Adjacent segment degeneration
Introduction
Lumbar spinal stenosis (LSS), one of the most common spinal disorders in the elderly, often results in low back pain, neurogenic claudication, and significant disability and impaired quality of life due to narrowing of the spinal canal and the pressure on nerves [1]. According to the literature, the incidence of LSS is as many as 38.8% of adults 60 years and older in the United States [2]. Traditionally, decompression with fusion and internal fixation has been the mainstay of surgical approaches to the management of symptomatic LSS [3-6]. However, some authors reported that it may be related to other problems such as serious trauma, transfusion requirement, pseudarthrosis as well as higher morbidity and mortality for elderly patients [7-10], especially adjacent segment degeneration [11-17]. In order to overcome these deficiencies associated with fusion surgery, an interspinous process device-Coflex system (Paradigm Spine, LLC, New York) was developed as a possible alternative to spinal decompression with posterolateral fusion and instrumentation [18-20]. Although the encouraging results of Coflex have been widely reported in the past a few years [21-24], there is still controversy of the long-term benefit of this procedure. High complication such as prosthesis loosening and spinous process fracture, reoperation rate, and costs with poor outcomes were also mentioned in the literature [25-27]. Is the interspinous Device-Coflex outdated in the treatment of LSS? The purpose of the present study is to evaluate whether Coflex implantation following spinal decompression provided better clinical outcomes compared with traditional decompression with pedicle screws fixation and fusion for symptomatic lumbar spinal stenosis through mid-term follow-up.
Materials and Methods
Clinical data
A prospective cohort study was conducted in our institute between June 2007 and June 2010. 100 consecutive patients with symptomatic degenerative LSS at L4/5 were recruited in the study. They were randomly divided into 2 groups: 50 patients were placed in the study group who were offered spinal decompression with Coflex implantation at the affected level, while 50 patients were placed in the comparison group who were treated decompression with pedicle screws fixation and interbody fusion. There were 29 males and 21 females with an average age of 57.6 ± 5.9 years (range, 48-70 years) in Coflex group. The ratio of males to females was 28:22 with an average age of 59.0 ± 6.7 years (range, 50-73 years) in fusion group. The preoperative data in the two groups is illustrated in Table 1.
| Title | Coflex Group | Fusion Group | p value | |
|---|---|---|---|---|
| Cases | Male | 29 | 28 | - |
| Female | 21 | 22 | - | |
| Age | 57.6 ± 5.9 (48-70) | 59.0 ± 6.7 (50-73) | >0.05 | |
| Follow-up period | 7.02 ± 0.34 | 7.62 ± 0.18 | >0.05 | |
Table 1: The general data of the present study.
Inclusion criteria: (1) Symptomatic LSS with obvious low back pain, intermittent claudication, or sciatica. (2) After 3 months’ conservative treatment still invalid. (3) Imaging examination confirmed to be LSS; (4) Affected segment (L4/5) with or without lumbar disc herniation or slight spondylolisthesis; (5) Without degeneration or instability of adjacent segments (L3/4, L5/S1).
Exclusion criteria: (1) Having a history of lumbar surgery. (2) Lumbar spine trauma, infection scoliosis, kyphosis, or ankylosing spondylitis. (3) Spondylolisthesis over II degrees or spondylolysis. (4) Adjacent segments (L3/4, L5/S1) degeneration or instability. (5) Severe osteoporosis.
Surgical technique
The Coflex group (decompression with Coflex implantation): Patients were operated under general anesthesia and in prone position. C-arm was used to determine L4/5 level before operation in everyone. A 4 cm-length-incision was chosen and paraspinal muscle separation was performed through a standard posterior midline approach in all the patients. Supraspinal Ligament was carefully separated to one side by sharp dissection. The interspinous ligament was dissected and excised. Partial laminotomy, excision of hypertrophic ligamentum flavum were performed to decompress the stenotic level with carefully protecting bilateral joint facet joints. Discectomy was also done if a herniation was confirmed. Then a suitable size Coflex was implanted at the interspinous of L4/5 after measurement as deep as possible so that the vertex of shape U was in the same line with the joint facet joints. The wings of the Coflex were clamped using the manufacturer’s forceps so that it was seated snugly. Satisfactory placement of the implant and adequate segmental sagittal alignment were ensured under C-arm image. Then the wound was closed routinely after placement of a closed suction drain.
The fusion group (decompression with pedicle screws fixation and interbody fusion): Anaesthesia and body position of the patients were the same as those of Coflex group. A posterior median incision of 4-5 cm long was chosen and paraspinal muscles were separated from the surface of spinous process and lamina, exposing both sides’ lamina and facet joints. Pedicle screws were placed in both sides of L4 and L5 under the monitoring of C-arm. Decompression was performed by bilateral laminectomy and hypertrophic ligamentum flavum resection, as well as enlargement of nerve root canal. After insertion of a cage with allograft bone, two rods were installed. A closed suction drain was placed routinely before the wound was closed.
Postoperative care
All the patients in both groups received similar postoperative care. They were allowed to ambulate as tolerated from the next postoperative day. Early return to activities was encouraged after surgery. The drainage was pulled out after 48 hours postoperative and the flow rate was less than 30 ml.
Clinical outcome assessment
Clinical outcome scores were assessed preoperative and at the last follow-up postoperative using the Japanese Orthopaedic Association (JOA) score, Oswestry disability index (ODI), 100 mm visual analogue scale (VAS) back pain and leg pain, and short form- 36 (SF-36). Operation time, intraoperative blood loss, ambulation time, and hospitalization days were also compared between the two groups. Complications were statistics and analysis in the two groups, respectively.
Radiological assessment
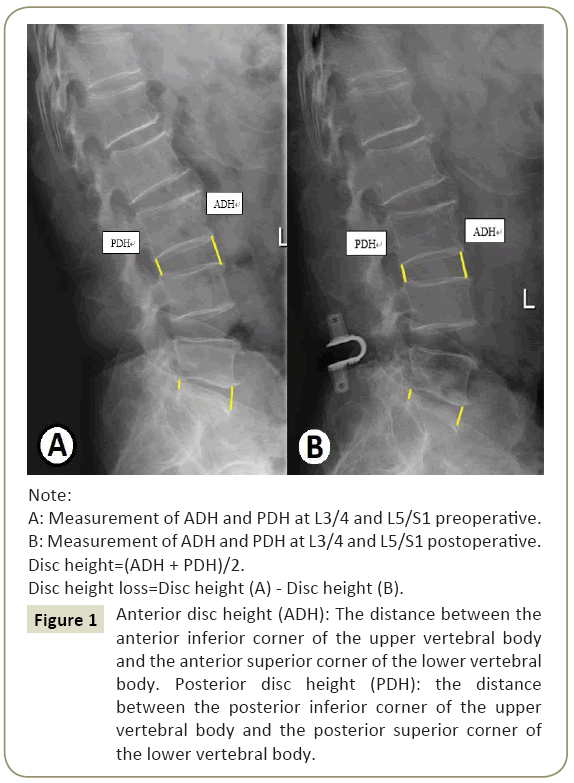
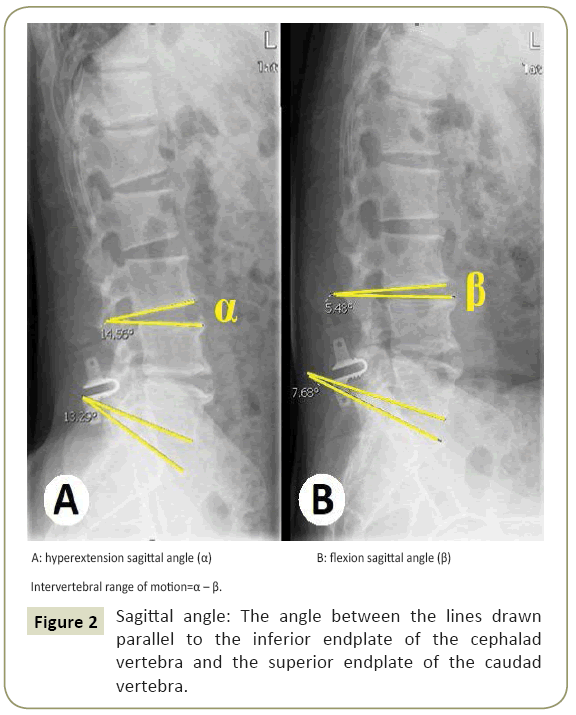
All the patients underwent lumbar spine radiographs including standardized, erect antero-posterior (AP), lateral, dynamic (hyperextension and flexion lateral) position and magnetic resonance imaging (MRI) examination preoperative and postoperative. The observer, who did not participate in surgeries, took all the measurements using the Carestream PACS system (Ver. 11.0, Carestream Health, Inc., Rochester, New York, 2008). Disc height was calculated by taking the mean of the anterior and poste rior disc heights at the level in question. Anterior disc height was calculated as the distance between the anterior inferior corner of the upper vertebral body and the an terior superior corner of the lower vertebral body. Like wise, posterior disc height was calculated as the distance between the posterior inferior corner of the upper verte bral body and the posterior superior corner of the lower vertebral body (Figure 1). Disc height loss was calculated by the difference between preoperative and the last follow-up postoperative disc heights. Sagittal angle was measured by determining the angle subtended between the lines drawn parallel to the inferior endplate of the cephalad vertebra and the superior endplate of the caudad vertebra. Intervertebral range of motion (ROM) was calculated by the difference between hyperextension and flexion sagittal angles (Figure 2). Increment of intervertebral ROM was calculated by the difference between the last follow-up postoperative and preoperative intervertebral ROMs. Intervertebral disc degeneration at L3/4 level and L5/ S1 level was also evaluated by Pfirrmann Classification [28] preoperative and at the last follow-up postoperative based on MRI.
Figure 1: Anterior disc height (ADH): The distance between the anterior inferior corner of the upper vertebral body and the an terior superior corner of the lower vertebral body. Posterior disc height (PDH): the distance between the posterior inferior corner of the upper verte bral body and the posterior superior corner of the lower vertebral body.
Statistical analysis
Statistical analysis was performed using SPSS soft package (Ver. 16.0, SPSS Inc., Chicago, IL, USA). One-way ANOWA was performed to compare operation time, intraoperative blood loss, ambulation time and hospitalized days between the two groups. A paired t-test was performed to compare the last follow-up JOA, ODI, VAS (back pain and leg pain), and SF-36 scores with the respective preop erative scores in both groups. Student- Newman-Keuls (SNK) technique was used to adjust for multiple comparisons. Mixed model analysis was performed to compare the improvement in JOA, ODI, VAS-back pain and leg pain, and SF- 36 scores between Coflex group and fusion group. Preoperative and postopera tive radiological measurements including disc height loss and increment of intervertebral ROM were compared within the two groups by using repeated measures ANOVA. SNK technique was used to adjust for multiple comparisons. Chi square test was used to compare the difference of Pfirrmann grade changes and complication rates between Coflex group and fusion group. A p-value of <0.05 was considered as statistically significant.
Results
Clinical outcome assessment
All patients in the two groups were followed up. The average follow-up period was 7.02 ± 0.34 years in Coflex group and 7.62 ± 0.18 years in fusion group, respectively. There was no statistically significant difference between the two groups (P>0.05). The operation time, intraoperative blood loss, ambulation time and hospitalization days in the two groups are illustrated in Table 2. There were statistically significant differences between the two groups (P<0.01).
| Title | Coflex Group | Fusion Group | p value |
|---|---|---|---|
| Operation time (min) | 54.33 ± 12.17 | 99.48 ± 24.56 | <0.001 |
| Intraoperative blood loss (ml) | 74.74 ± 23.33 | 184.10 ± 47.98 | <0.001 |
| Ambulation time (day) | 2.30 ± 0.46 | 3.79 ± 0.76 | <0.001 |
| Inpatient days (day) | 5.61 ± 1.13 | 8.28 ± 0.68 | <0.001 |
Table 2: The comparisons of the operation times, intraoperative blood loss, ambulation time, and inpatient days.
Clinical outcome scores
The clinical outcome scores are illustrated in Table 3. The mean JOA, ODI, VAS-leg pain, VAS-back pain and SF-36 scores in both Coflex group and fusion group showed significant improvement at the last follow-up as compared with preoperative scores (p<0.001). However, there were no statistically significant differences between Coflex group and fusion group in the mean improvement in JOA score (p=0.317), ODI score (p=0.159), VASleg pain score (p=0.295), VAS-back pain score (p=0.276), and SF- 36 score (p=0.603).
| Groups | JOA | ODI | VAS-leg pain | VAS-back pain | SF-36 | |
|---|---|---|---|---|---|---|
| Coflex group | Pre-op | 11.84 ± 2.45 | 41.94 ± 3.26 | 7.33 ± 1.08 | 6.89 ± 1.63 | 32.83 ± 4.65 |
| Post-op | 25.87 ± 2.06 | 4.58 ± 1.77 | 1.92 ± 0.62 | 1.22 ± 0.52 | 65.94 ± 4.13 | |
| P value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| Fusion group | Pre-op | 11.00 ± 2.01 | 42.92 ± 2.10 | 7.41 ± 0.93 | 7.44 ± 1.17 | 33.35 ± 4.13 |
| Post-op | 24.23 ± 3.27 | 4.66 ± 1.45 | 2.30 ± 0.97 | 1.35 ± 0.37 | 65.84 ± 4.03 | |
| P value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| Coflexgroup improvement | 14.02 ± 3.46 | -37.35 ± 3.48 | -5.41 ± 1.27 | -5.65 ± 1.48 | 33.12 ± 5.66 | |
| Fusion group improvement | 13.23 ± 3.78 | -38.25 ± 2.68 | -5.10 ± 1.44 | -5.89 ± 1.66 | 32.49 ± 5.18 | |
| P value | 0.317 | 0.159 | 0.295 | 0.276 | 0.603 | |
Table 3: The clinical outcomes scores of JOA, ODI, VAS and SF-36.
Radiological measurements
The mean height of adjacent segment disc was decrease in both Coflex group and fusion groups postoperatively. The mean height loss was 1.78 ± 0.70 mm at L3/4 level and 1.48 ± 0.38 mm at L5/ S1 level in Coflex group, while the mean height loss was 4.30 ± 0.87 mm at L3/4 level and 2.69 ± 0.49 mm at L5/S1 level in fusion group (Table 4). There was statistically significant difference between the two groups (P<0.01). The adjacent segment disc activities were increased in both Coflex group and fusion group. The mean sagittal angle showed an overall increase of 3.05 ± 1.30 degrees at L3/4 level and 3.04 ± 1.24 degrees at L5/S1 level in Coflex group. There was also a significant sagittal angle increase of 4.03 ± 0.34 degrees at L3/4 level and 4.01 ± 0.33 degrees at L5/S1 level in fusion group. There was statistically significant difference between the two groups (P<0.01) (Table 4).
| Levels | Coflex Group | Fusion Group | p value | |
|---|---|---|---|---|
| Disc height decrease | L3/4 level | 1.78 ± 0.70 | 4.30 ± 0.87 | <0.01 |
| L5/S1 level | 1.48 ± 0.38 | 2.69 ± 0.49 | <0.01 | |
| Adjacent segments ROM increment | L3/4 level | 3.05 ± 1.30 | 4.03 ± 0.34 | <0.01 |
| L5/S1 level | 3.04 ± 1.24 | 4.01 ± 0.33 | <0.01 | |
Table 4: Radiological measurements of disc height decrease (mm) and adjacent segments ROM increment (degree).
At the last follow-up, the upper and lower adjacent segment degeneration was evaluated using Pfirrmann grading system in both Coflex group and fusion group (Table 5). There were 7 patients progressed to grade IV from grade II or grade III at L3/4 level, 11 patients progressed to grade IV and one patient progressed to grade V at L5/S1 level in Coflex group. There were 15 patients progressed to grade IV at L3/4 level, 19 patients progressed to grade IV and 6 patients progressed to grade V at L5/S1 level in fusion group. There were statistically significant differences between the two groups at L3/4 level (p=0.019<0.05) and L5/S1 level (p=0.008<0.05), respectively.
| Grade | Coflex group | Fusion group | ||||||
|---|---|---|---|---|---|---|---|---|
| L3/4 | L5/S1 | L3/4 | L5/S1 | |||||
| Pre-op | Post-op | Pre-op | Post-op | Pre-op | Post-op | Pre-op | Post-op | |
| Grade I | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Grade II | 15 | 10 | 6 | 5 | 6 | 0 | 7 | 2 |
| Grade III | 35 | 33 | 40 | 29 | 44 | 35 | 33 | 13 |
| Grade IV | 0 | 7 | 4 | 15 | 0 | 15 | 9 | 28 |
| Grade V | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 7 |
| L3/4: p=0.019<0.05; L5/S1: p=0.008<0.05 | ||||||||
Table 5: Adjacent intervertebral disc degeneration according to Pfirrmann grading system.
Complications
Surgical complications were found 4 cases (8%) in Coflex group and 3 patients (6%) in fusion group, respectively. The incidence of complications was no statistically significant deferent between the two group (p=0.695). In Coflex group, there were two patients with spinous process fracture on L4, one patient with L4/5 recurrent stenosis and disc herniation, one patient with symptomatic L5/S1 disc herniation. Revision was performed on three patients with pedicle screws fixation and transforaminal interbody fusion except the one who was confirmed L4 spinous process fracture 6 months after surgery because of low back pain. After 3 months conservative therapy, the patient felt no longer pain and the radiological examination showed the fracture healed. During the follow-up period, there were still another 6 patients who were confirmed partial bone absorption of L4 spinous process, including 4 patients with Coflex loosening and slightly displacement. Nevertheless, observing without any treatment for the 6 patients because of no complaints at all. In fusion group, two patients were conformed to adjacent segment disease (ASD) at L3/4 level and one patient was occurred disc herniation and spinal stenosis at L5/S1 level. All the three patients underwent secondary revision surgery.
Discussion
Traditional decompression with posterior fusion is the primary procedure for the treatment of symptomatic LSS. The aim is to relieve clinical symptoms without considering the problem of fixed segment movement. Long-term follow-up reveals adjacent segment ROM increased to compensate for the lost ROM of the fixed segment, resulting in ASD [13-15,29-33]. Following improved knowledge of lumbar motion function, surgeons now consider how to treat lumbar degenerative disease while maintaining ROM, and dynamic stabilization has been developed and accepted. New materials and techniques have led to the development of many non-fusion techniques and devices, such as: nucleus replacement, artificial disc, interspinous process devices, and posterior dynamic stabilization. A systematic review comparing fusion with non-fusion techniques showed that nonfusion techniques-maintained ROM at the surgical level, had less side-effect on the adjacent level than fusion [34,35].
Coflex (Paradigm Spine, LLC, New York), a kind of dynamic interspinous Device, was first introduced by the French orthopedic surgeon Jacques Samani as an alternative to fusion in 1994. Since then, the device has been used in various degenerative spinal conditions [21-24,36-38]. Although it was initially developed as a motion-preserving alternative used to treat various lumbar degenerative disorders, long-term studies from Europe suggested that the subset of patients with spinal stenosis and Grade I spondylolisthesis experienced the most significant improvement. However, high level evidence on its clinical efficacy and indications remains limited. A multicenter randomized and controlled clinical research of Coflex has been approved by FDA as an adjunct to fusion but is not approved as a stand-alone spacer in USA [21].
In the present study, we compared the clinical results between Coflex implantation and fusion after spinal decompression in treatment of symptomatic LSS. It showed that Coflex group had the same good clinical efficacy as fusion group in JOA score, ODI, VAS-leg pain, VAS-back pain, and SF-36 score. There was no statistically significant difference between the two groups. However, Coflex group had the advantages of less trauma, less intraoperative blood loss, early ambulation and shorter hospitalization days compared with fusion group. The results of the present study were consistent with those of previous researches [21-23,36-39].
Based on radiological measurements, there was statistically significant difference between Coflex group and fusion group in the height loss of adjacent segment disc at the last follow-up. It showed that the mean height loss of adjacent segment disc in fusion group was much more than that in Coflex group at both L3/4 level and L5/S1 level. There was also statistically significant difference between the two groups in adjacent segment activity increase. There was more activity increase in fusion group than that in Coflex group at both L3/4 level and L5/S1 level. The stress in adjacent segment might increase much more in fusion group than that in Coflex group, which leading to postoperative ASD. Intervertebral disc degeneration in adjacent segments was observed in both groups by Pfirrmann classification at the last follow-up. However, there was significant difference between the two groups. Adjacent segment degeneration aggravation was found more cases and sever grade in fusion group than that in Coflex group. According to the results of this study, it can be concluded that decompression with Coflex implantation may have an advantage in preventing postoperative ASD compared with decompression with fixation and fusion in the treatment of symptomatic LSS.
The overall complication rate in the present study was lower than that in other researches [25-27]. One of the possible reasons was that the patient with instability or low-grade spondylolisthesis was excluded from Coflex group. Although there was seldom reported that the application of Coflex implantation developed significant improvement in the treatment of low-grade spondylolisthesis [21], we prefer to consider that Coflex is weak at stabling the intervertebral joint and cannot prevent intervertebral instability and further slipping. Therefore, no patient with intervertebral instability or low-grade spondylolisthesis was enrolled in Coflex group.
Among 4 cases of complications in Coflex group, there were 2 cases of spinous process fractures, which were all found at L4 and in early surgeries. The reasons for spinous process fracture might be that fenestration was a little bit larger, lamina near the base of L4 spinous process resection was a little bit more, and Colex implantation was not deep enough leading the supporting force acting on L4 spinous process increased. In the following surgeries, we paid more attention on fenestration, preserving lamina near the base of L4 spinous process, and implanting Coflex as deep as possible so that the arc vertex of the shape U was in the same line with joint facet joints. No spinous process fracture case was found in the following surgeries. Nevertheless, no complication of ADS was found in Colex group.
Conclusion
Previous research reported that additional Coflex implantation was safe but not beneficial in the treatment of symptomatic LSS [25]. In the present study, we found significant clinical improvements (JOA, ODI, VAS-back, VAS-leg and SF-36 scores) in patients of both groups after surgery. Although the improvements were not significantly different between the two groups, the implantation of Coflex had the advantage of less trauma, faster recovery and better lumbar function. It may play a role in reducing adjacent segments overactivity and ASD. Appropriate fenestration and lamina near the base of spinous process preservation may reduce complication as well as improve the effectiveness. Coflex implantation may be a better choice in avoiding fusion and its associated problem in the treatment of symptomatic LSS, and fusion surgery can still be a remedy for the failure of a non-fusion surgery. The limitation of this study is that the number of cases was small and the follow-up period was not long enough. Further research is needed prior to wide application.
Acknowledgements
The authors thank other members in Department of Orthopedics in Guangdong General Hospital, Guangdong Academy of Medical Sciences, Drs. Shiqiang Zhan, Shixing Zeng, Yongxiong Huang, Shuaihao Huang, Dan Xiao, and Yuhong Ke, who participated partly in this survey. Additionally, Dr. Liangze Wang made contributions to this study in data collection and statistics.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Competing and Conflicting Interests
The authors declare no conflict of interests concerning the materials and methods used in this study or the findings specified in this paper.
References
- Lin SI, Lin RM, Huang LW (2006) Disability in patients with degenerative lumbar spinal stenosis. Arch Phys Med Rehabil87: 1250-1256.
- Kalichman L, Cole R, Kim DH, Li L, Suri P, et al. (2009) Spinal stenosis prevalence and association with symptoms: the Framingham Study.Spine J9:545-550.
- Turner JA, Ersek M, Herron L, Deyo R (1992) Surgery for lumbar spinal stenosis attempted meta-analysis of the literature. Spine17: 1-8.
- Hansraj KK, O'Leary PF, Cammisa FP Jr, Hall JC, Fras CI, et al. (2001) Decompression, fusion, and instrumentation surgery for complex lumbar spinal stenosis. ClinOrthopRelat Res384: 18-25.
- Trouillier H, Birkenmaier C, Rauch A, Weiler C, Kauschke T, et al. (2006) Posterior lumbar interbody fusion (PLIF) with cages and local bone graft in the treatment of spinal stenosis. Acta OrthopBelg 72:460-466.
- Watanabe K, Yamazaki A, Morita O, Sano A, Katsumi K, et al. (2011) Clinical outcomes of posterior lumbar interbody fusion for lumbar foraminal stenosis:preoperative diagnosis and surgical strategy. J Spinal Disord Tech24: 137-141.
- Deyo RA, Cherkin DC, Loeser JD, Bigos SJ, Ciol MA (1992) Morbidity and mortality in association with operations on the lumbar spine the influence of age, diagnosis, and procedure. J Bone Joint Surg Am 74:536-543.
- Deyo RA, Martin BI, Kreuter W, Jarvik JG, Angier H, et al. (2011) Revision surgery following operations for lumbar stenosis. J Bone Joint Surg Am93: 1979-1986.
- Raizman NM, O’Brien JR, Poehling-Monaghan KL, Yu WD (2009) Pseudarthrosis of the spine. J Am AcadOrthopSurg17: 494-503.
- Suh SP, Jo YH, Jeong HW, Choi WR, Kang CN (2017) Outcomes of revision surgery following instrumented posterolateral fusion in degenerative lumbar spinal stenosis:A comparative analysis between pseudarthrosis and adjacent segment disease. Asian Spine J11: 463-471.
- Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine29: 1938-1944.
- Ghiselli G, Wang JC, Bhatia NN, Hsu WK, Dawson EG (2004) Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am86-A: 1497-1503.
- Lee CS, Hwang CJ, Lee SW, Ahn YJ, Kim YT, et al. (2009) Risk factors for adjacent segment disease after lumbar fusion. Eur Spine J18: 1637-1643.
- Xia XP, Chen HL, Cheng HB (2013)Prevalence of adjacentsegmentdegenerationafterspinesurgery: A systematic review and meta-analysis. Spine 38: 597-608.
- Hikata T, Kamata M, Furukawa M (2014) Risk factors for adjacent segment disease after posterior lumbar interbody fusion and efficacy of simultaneous decompression surgery for symptomatic adjacent segment disease. J Spinal Disord Tech27: 70-75.
- Epstein NE (2016) Older literature review of increased risk of adjacent segment degeneration with instrumented lumbar fusions. SurgNeurolInt7: S70-S76.
- Alentado VJ, Lubelski D, Healy AT, Orr RD, Steinmetz MP, et al. (2016) Predisposing characteristics of adjacent segment disease after lumbar fusion. Spine41: 1167-1172.
- Bono CM, Vaccaro AR (2007) Interspinous process devices in the lumbar spine. J Spinal Disord Tech20:255-261.
- Lee SH, Seol A, Cho TY, Kim SY, Kim DJ, et al. (2015) A systematic review of interspinous dynamic stabilization. ClinOrthopSurg7: 323-329.
- Gala RJ, Russo GS, Whang PG (2017) Interspinous implants to treat spinal stenosis. Curr Rev Musculoskelet Med10: 182-188.
- Davis RJ, Errico TJ, Bae H, Auerbach JD (2013) Decompression and Coflex interlaminar stabilization compared with decompression and instrumented spinal fusion for spinal stenosis and low-grade degenerative spondylolisthesis: two-year results from the prospective, randomized, multicenter, Food and Drug Administration Investigational Device Exemption trial. Spine 38: 1529-1539.
- Musacchio MJ, Lauryssen C, Davis RJ, Bae HW, Peloza JH, et al. (2016) Evaluation of decompression and interlaminar stabilization compared with decompression and fusion for the treatment of lumbar spinal stenosis: 5-year follow-up of a prospective, randomized, controlled trial. Int J Spine Surg10: 6-15.
- Bae HW, Davis RJ, Lauryssen C, Leary S, Maislin G, et al. (2016) Three-year follow-up of the prospective, randomized, controlled trial of Coflex interlaminar stabilization vs instrumented fusion in patients with lumbar stenosis. Neurosurgery79: 169-181.
- Li AM, Li X, Yang Z (2017) Decompression and Coflex interlaminar stabilisation compared with conventional surgical procedures for lumbar spinal stenosis: A systematic review and meta-analysis. Int J Surg40: 60-67.
- Richter A, Schütz C, Hauck M, Halm H (2010) Does an interspinous device (Coflex) improve the outcome of decompressive surgery in lumbar spinal stenosis? One-year follow up of a prospective case control study of 60 patients. Eur Spine J19: 283-289.
- Epstein NE (2012) A review of interspinous fusion devices: High complication, reoperation rates, and costs with poor outcomes. SurgNeurolInt3: 7-14.
- Zang L, Du P, Hai Y, Su QJ, Lu SB, et al. (2013) Device related complications of the Coflex interspinous process implant for the lumbar spine. Chin Med J126: 2517-2522.
- Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine26: 1873-1878.
- Lee JC, Kim Y, Soh JW, Shin BJ (2014) Risk factors of adjacent segment disease requiring surgery after lumbar spinal fusion: comparison of posterior lumbar interbody fusion and posterolateral fusion. Spine39: E339-E345.
- Masevnin S, Ptashnikov D, Michaylov D, Meng H, Smekalenkov O, et al. (2015) Risk factors for adjacent segment disease development after lumbar fusion. Asian Spine J9: 239-244.
- Kim JY, Ryu DS, Paik HK, Ahn SS, Kang MS, et al. (2016) Paraspinal muscle, facet joint, and disc problems: Risk factors for adjacent segment degeneration after lumbar fusion. Spine J16: 867-875.
- Scemama C, Magrino B, Gillet P, Guigui P (2016) Risk of adjacent-segment disease requiring surgery after short lumbar fusion: Results of the French Spine Surgery Society Series. J Neurosurg Spine 25: 46-51.
- Yamasaki K, Hoshino M, Omori K, Igarashi H, Nemoto Y, et al. (2017) Risk factors of adjacent segment disease after transforaminal inter-body fusion for degenerative lumbar disease. Spine42: E86-E92.
- Schmoelz W, Erhart S, Unger S, Disch AC (2012) Biomechanical evaluation of a posterior non-fusion instrumentation of the lumbar spine. Eur Spine J21: 939-945.
- Wang JC, Arnold PM, Hermsmeyer JT, Norvell DC (2012) Do lumbar motion preserving devices reduce the risk of adjacent segment pathology compared with fusion surgery? A systematic review. Spine37: S133-S143.
- Park SC, Yoon SH, Hong YP, Kim KJ, Chung SK, et al. (2009) Minimum 2-year follow-up result of degenerative spinal stenosis treated with interspinous U (Coflex). J Korean NeurosurgSoc46: 292-299.
- Cabraja M, Abbushi A, Woiciechowsky C, Kroppenstedt S (2009) The short- and mid-term effect of dynamic interspinous distraction in the treatment of recurrent lumbar facet joint pain. Eur Spine J18: 1686-1694.
- Celik H, Derincek A, Koksal I (2012) Surgical treatment of the spinal stenosis with an interspinous distraction device: Do we really restore the foraminal height? Turk Neurosurg22: 50-54.
- Kumar N, Shah SM, Ng YH, Pannierselvam VK, Dasde S, et al. (2014) Role of Coflex as an adjunct to decompression for symptomatic lumbar spinal stenosis. Asian Spine J8: 161-169.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences