Effects of Transcranial Direct Current Stimulation (tDCS) on Chronic Pain in Spinal Cord Injured Patients
Anna Maria Cortese, Alexander Nowicky, Luis López de Heredia, and Maurizio Belci
DOI10.21767/2471-8173.100024
Anna Maria Cortese1*, Alexander Nowicky2, Luis López de Heredia3, and Maurizio Belci3
1Department of Neurorehabilitation, I.R.C.C.S. San Camillo Hospital, via Alberoni 70, 30126, Venice, Italy
2Deparment of Clinical Sciences, College of Health and Life Sciences, Brunel University London, Uxbridge UB8 3PH, UK
3Stoke Mandeville Hospital/National Spinal Injuries Centre, Aylesbury, Oxfordshire, UK
- *Corresponding Author:
- Anna Maria Cortese
Department of Neurorehabilitation, I.R.C.C.S. San Camillo Hospital, via Alberoni 70, 30126, Venice, Italy
Tel: +44 1895 274000
E-mail: annamariacortes1982@libero.it
Received date: October 25, 2016; Accepted date: March 17, 2017; Published date: March 22, 2017
Citation: Cortese AM, Nowicky A, de Heredia LL, et al. Effects of Transcranial Direct Current Stimulation (tDCS) on Chronic Pain in Spinal Cord Injured Patients. Spine Res 2017, 3:1. doi:10.21767/2471-8173.10002
Abstract
Introduction: Pain following spinal cord injury (SCI) is notoriously difficult to manage and often refractory to treatment. Novel approaches, such as non-invasive brain stimulation, targeting central mechanisms associated with chronic pain, have shown early promise as a safe treatment in various patient groups, including spinal cord injury. To date the number of small clinical trials using non-invasive brain stimulation to treat chronic pain in SCI has produced mixed results. We report here the findings of a UK based trial examining the effects of anodal transcranial direct current stimulation (TdCs) administration on pain in spinal injury patients.
Methods: Sixteen spinal injury patients from the National Spinal Injury Centre, Stoke Mandeville Hospital, Aylesbury, UK participated in a single centre, double blind randomized control trial. Patients were randomly allocated to either the active (n=8) or sham (n=8) treatment groups. tDCS was administered by electrodes with anode placement over the dominant M1 and the cathode electrode over the contralateral supraorbit scalp area. Subjects received either active (2 mA anodal current) or sham tDCS for 20 min daily treatment for 5 consecutive days with the dose based on previously reported chronic pain studies in spinal cord injury patients. A mixed ANOVA was used to evaluate both tDCS treatment and time effects on validated assessment measures for pain and depression up to 2 weeks following treatment intervention.
Results: No adverse effects of the treatment were observed in this study, nor were there any significant differences between groups in rating perception of stimulation. While treatment appeared to have reduced group pain scores on a visual analogue scale [VAS], there were no statistically significant differences between active and sham treatment groups when re-examined in the 2 week follow up.
Conclusion: There were some reductions in self-assessed VAS pain score in our small group of SCI patients during treatment in both the sham and active tDCS and at two weeks’ post treatment. However, our study appears to indicate only a placebo-like effect of tDCS on chronic pain in SCI, and not one attributed to the active, anodal stimulation over motor cortex. We also did not observe any significant effects over time or treatment for an assessment of neuropathic pain. We observed some trends of non-significant reduction in some of selfassessed pain scores measures, however, these are inconclusive. Studies of clinical efficacy of pain treatment by tDCS in spinal cord injury should therefore be conducted on a larger scale, and with a longer follow up period to address the limited evidence available.
Keywords
Spinal cord injury; Pain; Neurostimulation; tDCS
Introduction
Pain is a common secondary complication following spinal cord injury (SCI) affecting the bio-psycho-social aspect of patient’s life [1]. In addition to loss of mobility, chronic pain is one of the most serious consequences of SCI, and the most persistent symptom associated with spinal cord injury [2]. Pain also directly contributes to disability by limiting participation in rehabilitation and return to work [3]. Pain may be continuous or it can worsen following SCI, it has also been observed that patients reporting neuropathic pain 3-6 month following SCI are likely to continue experiencing it at 3-5 years, in addition, pain has a broad impact on physical, emotional, cognitive and social functioning that needs to be evaluated and addressed in any management plan [4]. Achieving optimal pain reliefs reliant on an accurate identification of the type of pain present [5] as it has been increasingly recognized that pain following SCI may be due to a complex combination of changes at a various nervous system levels [6].
In a high percentage of cases, pain following SCI is refractory to treatment approaches which include: drug interventions (i.e. anticonvulsants, analgesics, opioids, anti-nflammatory, antidepressants), surgical approaches, physical medicine and rehabilitation. However, despite various treatments, evidence from clinical trials indicates that satisfactory (50% pain reduction or more) pain relief is at best obtained in only one third of individuals [7]. In conclusion, pain in SCI patients is complex, the mechanism is poorly understood and it is further complicated by the psychosocial impact of the nature of injury.
Treatment and management modalities do not work in isolation and need to be combined with pharmacological treatments, physical therapy and psychological input in specialist centers. More research needs to be conducted in novel experimental therapies with emphasis on improving patient’s quality of life after SCI [8]. Non-invasive brain stimulation (NIBS) techniques have shown early promise in treating chronic pain, and moreover shown to be well tolerated and safe [2,8]. The proposed mechanism of action suggests that, like direct cortical stimulation of motor cortex, they alter subcortical circuits associated with persistent pain [9]. Based, on some success with these methods in pain trials, it is suggested that these may act by modulating neuroplasticity activity of central pain mechanisms [10,11]. Among the NIBS techniques used to treat pain, both repetitive transcranial magnetic stimulation (Rtms) and transcranial direct current stimulation (Tdcs), have been trialed and earlier results have been the impetus for possible therapeutic treatment approaches for chronic pain following spinal cord injury [12]. Studies have shown that both methods may be effective in pain relief [11], but tDCS have key advantages over rTMS that have made it a more attractive application for pain relief. tDCS equipment is less expensive, much more portable, and commercially available devices enable potential selfadministration in an outpatient setting. tDCS applies continuous weak electrical current on the scalp and acts through inducing changes in the electrical properties of the neuronal membrane that can result in depolarization (anodal) or hyperpolarization (cathodal) of the stimulated area. Since some studies monitoring excitability changes in human motor cortex have demonstrated that changes in excitability outlast the application duration for several minutes to hours, possible synaptic effects may also be involved. Thus, application of tDCS over the motor cortex (M1) may modulate pain perception through indirect effects on pain modulating areas such as thalamic and subthalamic nuclei [13].
In the earlier RCT study by Fregni et al. [11], one week of daily 2 mA tDCS treatment over dominant M1 in SCI patient showed a significant reduction of pain for active treatment only. Although subjects were only evaluated for 16 days, the significant reductions in this treatment-resistant pain individuals suggested that tDCS may be an effective option for management of neuropathic pain in SCI patients [11]. In contrast a more recent study using a small cohort of patients utilizing a cross over design showed that tDCS did not provide any pain relief in subjects with neuropathic SCI pain out to 6 months post treatment [2].
In this additional feasibility study, we examined the possible therapeutic effects of 5 days anodal tDCS treatment on chronic pain in a small group of SCI patients admitted to spinal injury wards undergoing rehabilitation.
Methods
This study was a single centre, double blind, randomized, sham-controlled trial located at the national spinal injury centre (NSIC) at Stoke Mandeville Hospital (Aylesbury, UK). Inpatients were recruited from spinal injury wards and randomly assigned to either groups. At the outset of the study, sample size calculation, based on a Fregni study [12], anticipated 16 or more subjects per treatment groups. Participants were enrolled between August 2012 and May 2014 with the following inclusion criteria: moderate/severe pain assessed with the visual analogue scale (VAS) scoring pain perception of 4 or higher (moderate-severe intensity) and stable over 1 week at baseline, and on a stable pain treatment (medication and rehabilitation). Those excluded from the study were: affected from other neurological or neuropsychiatric diseases, including epilepsy, with a history of severe head injury, a history of unmanaged substance abuse and acute dermatological condition affecting the scalp. Group allocation was done sequentially by enrolment through an allocation list generated using online software (www.random.org). The study complied with the ethical standards of the Helsinki declaration was approved by local research ethics committee (Health Research Authority National Research Ethics, Bristol REC Centre, Bristol BS1 2NT UK). Participants provided written consent.
The study was structured in 3 phases following the initial recruitment: one week baseline, 5 days of daily treatment with tDCS, and a 2 week follow up. In addition to daily assessment of VAS pain, several other self-assessments were undertaken by each participant, as well as other outcome measures obtained by a blinded clinical assessor. Moreover, during the treatment week, participant’s vital signs (temperature, pulse rate, saturation and blood pressure) were monitored before and after the intervention but none of the participants exhibited any adverse effects that would warrant exclusion from further tDCS treatment. During the post-treatment follow up period, all assessments were obtained daily for the first 5 days, and then weekly for up to 2 weeks post treatment, including a weekly full clinical assessment of all outcome measures.
tDCS
Sham or anodal tDCS was applied by means of a programmable battery-operated constant current unit, (model-Neuroconn DC stimulator Plus®, Rogue Resolutions, Wales UK]. Stimulation was applied through carbon rubber electrodes inserted into sponge pockets (both 5 × 7 cm) soaked in isotonic saline and coated with conductive ultrasound gel to reduce scalp/hair impedance (<10 k Ohms). The anode (positive) electrode was centred over C3 or C4 [of the dominant hemisphere) which was first measured and marked on the head with indelible pen. Identification of M1 anode electrode placement was from Cz (vertex of 10-20 International System of Electroencephalography]in compliance with tDCS electrode placement guidelines, and typically 3 cm to 5 cm lateral to midline. The cathode was positioned over the contralateral frontal supraorbit. Electrodes were fixed securely and comfortably to the scalp with two elastic bandages. The tDCS stimulation was delivered for 5 consecutive days to each patient on the ward, while either sitting upright in bed or in a wheelchair between 9 am and 5 pm, accommodating patient’s timetable of daily rehabilitation activities.
For the real stimulation, 2 mA current intensity was applied for 20 minutes, with a ramp duration at onset/offset of 20 sec, (current density of 0.057 mA/cm2, total daily charge of 68.6 mC/cm2). Our rationale for location, electrode size, orientation and current strength was based on relevant earlier pain study which also used 2 mA current targeting the dominant primary motor cortical area [11]. For sham stimulation, 2 mA current was maintained for 30 sec following the same onset/offset rise time, (current density of 0.057 mA/cm2, total daily charge=1.7 mC/cm2). Thus, for the sham treatment, this duration was longer than previous sham stimulation duration parameters, but well below minimum duration reported to produce M1 excitability after effects [13].
Previous studies have identified that the use of short duration [10-20] of the target current is a suitable method of sham application, given that the perception of the electrically induced sensation of tingling and itchiness during application are rapidly habituating, so that it is difficult to identify sham or active conditions based on this sensation [13]. While we were aware of recent concerns about the sham integrity of 2 mA current, our study was a replication of pain relief and determined not to use a weaker intensity, but we monitored possible detection by patients as describe later. To ensure both operator and patient blinding, we utilized the study mode of the stimulation device, which required a 5 digit numerical code to be entered each day to initiate application. The set of unique numerical codes were pre-allocated according to the randomized treatment list by an independent researcher who was not involved in this study. During this mode of operation, only a countdown of stimulation duration was shown on the LCD display irrespective of type of stimulation. Thus, double blinding included, the operator, patients, and the clinician involved with assessments and was maintained throughout the statistical analysis. We also monitored daily reported sensations associated with the treatment and evaluated this using Likert scales (0-3 rating of sensation). In addition, at the end of the week, patients were also asked to rate how certain they were of the type of treatment received using a 5 point Likert scale: ([1] certain sham, [2] might be sham, [3] unsure either way[4] might be active, [5] certain active).
Outcome measures
Pain and depression measures used were the following selfassessed and combined patient and clinician assessments, which have been previously validated: VAS (10 cm Visual Analogue Scale), Leeds Assessment for Neuropathic Symptoms and Signs (LANSS, range 0-24), Mc Gill Pain Questionnaire (range 0 to 78, the higher the score the higher the pain), Brief Pain Inventory (BPI)-severity (range 0 to 10) and intensity (range 0 to 10), Clinical Global Impression of Change CGI-C scores range from 1 (very much improved) to 7 (very much worse), Patient Global Impression of change (PGIC) scale ( range 1 no changes after the treatment to 7 a great deal better after treatment), and Beck Depression Inventory (BDI) (range 0 to 63 with score 0-13 no depression, 14-19 mild depression, 20-29 moderate depression, 30-63 severe depression).
Statistical analysis
Data were analysed using SPSS (Statistical Package for Social Science for windows version 20, IBM). Following the main statistical analysis of the study, identification of the two treatment group allocations was revealed. One participant (A7) in the anodal tDCS treatment group was not given the LANSS Neuropathic pain for the study at baseline, and for others there were some missed assessments at various time points during the follow up monitoring period, which represented about 20% of the complete data set. Normality of the data was assessed using the Shapiro-Wilks test and therefore parametric statistics was determined appropriate here. Evaluation of Likert scale assessment of perception, type of sensation, and treatment detection was by independent samples t-tests. In order to compare baseline characteristics between the two groups in this study we used independent samples t-tests for patient characteristics and assessment pain scores. A mixed factors ANOVA was used to examine the interaction effect of tDCS treatment (between groups factor) and time (within factor). Levene’s test for equality of variance and Mauchly’s sphericity test were also undertaken and where necessary sphericity adjustment to the degrees of freedom using Greenhouse-Geisser adjustments are reported. Statistics reported here include the exact p value and partial eta squared (ÃÆÃâ Ãâàp2) for F tests in SPSS. Significance was set at p<0.05, and post hoc comparisons between group were undertaken using a Sidak correction. The analysis was undertaken on raw assessment scores across baseline, treatment days and up to 2 weeks post treatment. Group mean and standard deviations and 95% Confidence intervals (CI) are reported in the text.
Results
Of the 18 patients recruited for this study two dropped out in the early stages, one completing 5 days of treatment, and the other dropped out after the first day of treatment. Therefore, data are provided on 16 subjects, with 8 in each of the two treatment groups. The majority of the participants in this study were male with only three females (sham (1) and active (2)) participants. The baseline characteristics of participants are shown in Table 1. Notable differences in the composition of patients according to AIS classification are also noted: Sham treatment group, 5 complete (AIS A), 3 incomplete (AIS B and D), and for Active treatment group, 2 complete, and 5 incomplete (AIS B, C and D). In terms of injury, both groups mainly consisted of those who had traumatic injury, and one in each group was diagnosed with transverse myelitis. Baseline comparisons between the two groups are shown in Table 2. T-tests revealed no significant differences between treatment group allocation, for age, time since injury, and most of the assessments, except for significant higher BPI pain intensity and severity scores for the sham treatment group.
| Patient | Treatment | Hand | Age | Gender | Months post injury |
AIS | Injury Level |
Type of Injury |
VAS pain |
LANSS | MGPQ | BDI |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| S1 [5] | sham | L | 28 | M | 125 | B | C5 | T | 8 | 19 | 59 | 35 |
| S2 [7] | sham | R | 33 | M | 9 | B | C6 | T | 5 | 17 | 6 | 18 |
| S3 [8] | sham | L | 40 | M | 12 | A | C8 | T | 3 | 12 | 34 | 6 |
| S4 [11] | sham | R | 51 | M | 7 | A | C4 | T | 8 | 19 | 40 | 29 |
| S5 [12] | sham | L | 38 | M | 23 | A | T4 | T | 7 | 19 | 53 | 27 |
| S6 [13] | sham | L | 33 | M | 72 | A | C4 | T | 8 | 11 | 51 | 32 |
| S7 [14] | sham | R | 52 | M | 302 | A | T10 | T | 9 | 5 | 57 | 4 |
| S8 [16] | sham | R | 42 | F | 3 | D | T4 | TM | 5 | 17 | 12 | 2 |
| A1[1] | active | R | 33 | 12.5 | A | T11 | T | 4 | 7 | 24 | 4 | |
| A2 [3] | active | R | 61 | M | 4 | C | C6 | T | 6 | 15 | 27 | 7 |
| A3 [4] | active | R | 60 | M | 5 | C | C5 | T | 6 | 9 | 36 | 22 |
| A4 [6] | active | R | 47 | M | 5 | D | C4 | T | 5 | 5 | 8 | 7 |
| A5 [9] | active | R | 29 | M | 4 | D | T4 | T | 6 | 23 | 43 | 47 |
| A6 [15] | active | R | 28 | F | 156 | A | T4 | T | 5 | 6 | 6 | 20 |
| A7 [17] | active | R | 57 | F | 4 | D | C4 | TM | 7 | - | 24 | 1 |
| A8 [18] | active | R | 67 | M | 5 | D | T2 | T | 6 | 12 | 48 | 11 |
Table 1 Baseline data for SCI patients in the study. American spinal injury association (ASIA) classification (A-D); injury: traumatic (T), transverse myelitis (TM), visual analog scale (VAS); The Leeds Assessment of Neuropathic Symptoms and Signs (LANSS)] Pain Scale; The McGill Pain Questionnaire (MGPQ): Beck depression inventory (BDI).
| Sham | 2mA tDCS | Mean Difference | T statistic | P | |
|---|---|---|---|---|---|
| Age in years | 39.6 (8.6) | 47.8 (15.8) | -8.125 | -1.28 | 0.221 |
| Time from injury (mo.) | 69.1 (103.2) | 24.4 (53.3) | 44.7 | 1.09 | 0.295 |
| VAS pain (1-10) | 6.4 (1.7) | 5.3 (1.4) | 1.087 | 1.4 | 0.183 |
| BDI (1-63) | 19.1 (13.5) | 14.8 (14.9) | 4.25 | 0.60 | 0.560 |
| BRF Pain Severity [0-10] |
6.5 (1.8) | 4.47 (0.92) | 1.99 | 2.76 | 0.015* |
| BRF Pain intensity (0-10) |
5.6 (2.2) | 3.2 (1.78) | 0.812 | 2.39 | 0.032* |
| MGPQ (0-76) | 37.3 (21.4) | 27.0 (15.1) | 13.4 | 1.34 | 0.202 |
| LANSS (0-24) | 14.8 (5.1) | 11.0 (6.4) | 3.88 | 1.29 | 0.212 |
VAS: visual analogue scale; BDI: Beck’s depression inventory; BRF Brief pain inventory; MGPQ: McGill pain questionnaire; LANSS: Lans assessment for neuropathic symptoms and signs
Table 2 Baseline assessments for the two treatment groups. Means and standard deviations are shown for the two treatment groups as well as independent t-tests results for comparison.
All patients tolerated the daily application of tDCS, with no adverse effects reported during the week of administration, or in the follow up period. Patients described the stimulation, irrespective of treatment, as mild tingling without pain, under one or both of the electrodes. There were no significant differences for ratings of stimulation sensation between groups, (Table 3). The detection of treatment type by the participants, obtained on the last day of administration, were 3.0 (1.5) for the sham and 4.0 (1.4) for the active, which were not significantly different (mean difference (-1.0; CI-2.57 to 0.57); t(14)=1.37; p=0.19).
| Perception of stimulation | Sham tDCS Group | 2 mA Anodal tDCS Group |
T-test (df=14) | P value |
|---|---|---|---|---|
| Itchiness (0-3) | 1.75(0.9) | 1.13(1.0) | 1.33 | 0.21 |
| Burning (0-3) | 1.38(0.74) | 1.13(1.25) | 0.48 | 0.63 |
| Tingling (0-3) | 1.75(1.1) | 0.75(0.5) | 1.82 | 0.09 |
| Pain (0-3) | 1.0(0.0) | 0.63(0.5) | 2.05 | 0.06 |
| Detection of type of tDCS treatment (1-5) |
3(1.5) | 4(1.4) | -1.37 | 0.19 |
Table 3 Perception and Detection of tDCS treatment: Rating of perception on last day of treatment on different types of sensation under one or both electrodes (0-no sensation to 3-strong sensation). Assessment treatment identification as sham or active using: (1) definitely sham, (2) might be sham, (3) unsure, (4) might be active, (5) definitely active.
VAS pain
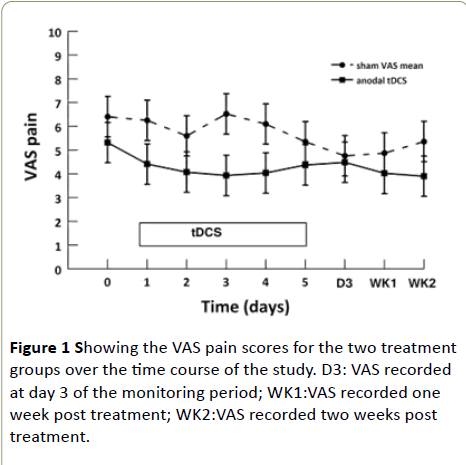
Figure 1 illustrates the VAS pain scores for the two treatment groups over the time course of the study. The baseline average VAS pain score was 6.4 (CI 5.2 to 7.6) for the sham group and 5.3 (CI 4.1 to 6.5) for the active group, respectively. The ANOVA revealed no significant differences between treatment groups, F(1.14)=0.96, p=0.34, ÃÆÃâ Ãâàp2=0.064, but a significant effect of time, F(5.5)=5.41, p=0.001, ÃÆÃâ Ãâàp2=0.28; while there was no significant interaction effect, F(5.5)=1.13, p=0.352, ÃÆÃâ Ãâàp2=0.075. In post hoc comparisons, for the main effect of time, there was a significant mean difference between baseline and two weeks post treatment, (1.75 [CI: 0.25 to 3.2]; p=0.016). At two weeks post treatment, the mean VAS pain scores was 4.4 (CI 2.4 to 6.5) for sham group and 3.8 (CI 1.76 to 5.8) for active group, respectively as showed in Figure 1.
Leeds assessment for neuropathic symptoms and signs (LANSS)
LANSS neuropathic pain scores at baseline for the sham (15.4 CI 10.4 to 20.5) and active group (11.0 CI 5.4 to 16.3) were similar to the LANSS scores at two weeks post treatment: the sham group (15.6 CI 8.7 to 22.5) and active group (9.0 CI 1.56 to 16.5), respectively. The ANOVA revealed no significant treatment effect, F (1.11)=1.72, p=0.22, ÃÆÃâ Ãâàp2=0.14, as well as no significant effect of time F(3.33)=0.24, p=0.87, ÃÆÃâ Ãâàp2=0.02, or interaction of treatment x time, F(3.33)=0.33, p=0.81, ÃÆÃâ Ãâàp2=0.03.
The McGill pain questionnaire
The mean McGill pain questionnaire (MCPQ) score at baseline was 37.3 (CI 22.4 to 52.2) for the sham group, and 27.0 (CI 13.0 to 41.0) for the active group, respectively. While at post 2 weeks, these scores were 38.3 (CI 22.6 to 53.9) for the sham group, and 23.6 (CI 9.0 to 38.3) for the active group. There was no significant effect of type of treatment on scores on the McGill Pain Questionnaire, F(1.13)=2.54, p=0.135, ÃÆÃâ Ãâàp2=0.16, nor a significant effect of time F(2.26)=0.96, p=0.40, ÃÆÃâ Ãâàp2=0.07, but the interaction of treatment × time was statistically significant, F(2.26)=3.58, p=0.042, ÃÆÃâ Ãâàp22=0.22
The brief pain inventory (BPI)
Severity: As noted at baseline, the brief pain inventory (BPI) score for severity was 6.5 (CI 5.3 to 7.8) for the sham group and 4.5 (CI 3.3 to 5.6) for the active group were significantly different (t=2.77, p=0.015). While at post two weeks, this score was 5 (CI 3.2 to 6.8) for the sham group and 4.3 (CI 2.6 to 6.0) for the active group. The ANOVA revealed no significant effect here: for treatment, F(1.13)=1.88, p=0.19, ÃÆÃâ Ãâàp2=0.13, however, a significant effect of time F(2.26)=3.89, p=0.033, ÃÆÃâ Ãâàp2=0.23, but a non-significant interaction of treatment × time F(2.26)=2.56, p=0.10, ÃÆÃâ Ãâàp2=0.16.
Intensity: At baseline the BPI score for intensity, for the sham group was 5.3 (CI 3.6 to 6.8) and 3.74 (CI 1.4 to 6.1) for the active group were significantly different (t=2.39, p=0.039). While at post two weeks, these were lower, with the sham group score of 3.7 (CI 1.4 to 6.1) and 3.0 (CI 0.83 to 5.2) for the active group. The ANOVA showed no significant effects of treatment, F(1.13)=1.36, p=0.26, ÃÆÃâ Ãâàp2=0.09, time, F(2.26)=1.58, p=0.22, ÃÆÃâ Ãâàp2=0.11, or interaction of treatment x time, F(2.26)=0.84, p=0.44, ÃÆÃâ Ãâàp2=0.06.
Clinical global impression of change (CGIC): The clinician’s impression of change in the pain using the CGIC was assessed at the end of the 5 days treatment with a mean of 2.7 (CI 1.9 to 3.6) for the sham group and 3.2 (CI 2.6 to 3.1) for the active group. At reassessment, two weeks later, these scores were 2.9 (CI 2.0 to 3.7) for the sham group and 2.4 (CI 1.8 to 3.1) for the active group respectively. The ANOVA for treatment, F[1.12]=0.68, p=0.42, ÃÆÃâ Ãâàp2=0.05, and time F(1.12)=0.012, p=0.74, ÃÆÃâ Ãâàp2=0.01, were not significant, however, there was a significant interaction of treatment x time F(1.12)=5.65, p=0.035, ÃÆÃâ Ãâàp2=0.32.
Patient Global Impression of change (PGIC): For the selfassessed patient impression of change (PGIC) the mean score was 3.1 (CI 1.4 to 4.8) for the sham, and 3.3 (CI 1.6 to 4.9) for the active group and hence were not significantly different at baseline. While at post two weeks, this was 3.13 (CI 1.4 to 4.8) for the sham, and 3.2 (CI 1.6 to 4.9) for the active group respectively. The ANOVA showed no significant effect of treatment, F(1.12)=0.18, p=0.66, ÃÆÃâ Ãâàp2=0.02, or time F(1.12)=0.48, p=0.5, ÃÆÃâ Ãâàp2=0.04, or interaction of treatment x time F(1.12)=0.12, p=0.74, ÃÆÃâ Ãâàp2=0.01.
Becks depression inventory (BDI): We also evaluated the mean BDI depression scores, which was 17.3 (CI 5.6 to 29) for the sham group and 14.9 (CI 4.0 to 25.8) for the active group and were not significantly different at baseline. At post two weeks these were 13.6 (CI 2.7 to 24.4) for the sham group and 15.1 (CI 5.0 to 25.3) for the active group respectively. The ANOVA revealed no significant effects of treatment, F(1.13)=0.026, p=0.87, ÃÆÃâ Ãâàp2=0.002, or time F(2.26)=3.012, p=0.067, ÃÆÃâ Ãâàp2=0.19, but a significant interaction of treatment × time F(2,26)=4.91, p=0.016, ÃÆÃâ Ãâàp2=0.27.
Discussion
The overall aim of this study was to examine whether 2 mA daily treatment with anodal tDCS produced a clinical significant reduction in chronic pain following SCI. Our findings did not show a treatment dependent difference in the main measure of self-reported VAS pain and other measures obtained post treatment in general. There was a reduction of 2 points on the VAS for the sham group and 1.5 points for the active group at two weeks post treatment observed in both groups sampled in this study. However, we noted some significant interaction effects with a small reduction in MGPQ scores for the active treatment, as well as small increase in both CGIC and PGIC.
Anodal tDCS of the motor cortex has been reported to increase the pain threshold and to provide relief from neuropathic pain [14]. One of the studies we used as reference for our experimental protocol was that of Fregni et al. [11] which evaluated a follow up period following 5 days of anodal tDCS for up to post 16 days. This study gave a strong indication that tDCS may be an effective treatment for central pain due to traumatic SCI, showing a reduction in mean pain of 37% at 16 days, post treatment for the active treatment only. In our study, we found that there was a significant reduction in VAS pain measures over the time of the study, but of only 31% (sham) and 28% (active) treatment, respectively. There was a non-significant reduction in pain ratings after 5 days of trial but similar for both the sham and active treatments.
Wrigley et al. [2] examined changes in neuropathic pain scores following 5 days of similar dosage for up to one year, and did not find a statistically significant reduction in overall pain intensity in patients with neuropathic pain following SCI. They suggested that the reason for the lack of tDCS efficacy was the prolonged period since injury onset in their patients, since a negative correlation between pain intensity changes after tDCS treatment and duration of SCI had already been noted by the Fregni et al. [11]. Wrigley et al. [2] suggested the possibility that central changes resulting from neuropathic SCI pain had become consolidated, so that tDCS could not modulate the central pain related system.
In our study, the time from injury varied from patient to patient, with some as short as 3 months and some as long as 325 months, but overall there was no group difference at baseline, despite, the sham group average time from injury was 69 months while for the active group this was 24 months. This difference in the time from the injury between the groups resulted from the randomization process but in order to examine this impact on findings, other studies should consider shorter times since injuries for future evaluations of this form of treatment. Our results albeit of a small sample here, do show that pain perception was diminished in both groups overall, therefore, the time from injury should not be correlated with the reduction of pain in our patients unlike the Fregni et al. [11] and Wringley et al. [2] trials.
Additionally, we noted a reduction in self-reported pain measures (VAS) during the active period for both the sham and the active treatment. That finding could be linked to the placebo effect associated with the tDCS administration. It is worth considering, therefore, the impact of placebo treatments and their potential effects in pain relief since its impact may be particularly important for non-invasive brain stimulation (NIBS) studies. In our trial, there was no differences between the two groups in terms of detection of the type of treatment. Of note in this regard, is a recent study which investigated the placebo effects of tDCS on depression demonstrating that tDCS reinforces brain networks activated by the expectation of therapeutic benefit, in other words, tDCS fortifies the placebo response to which it may, in part, contribute. Therefore, the investigators suggested that tDCS and placebo pills should be combined to increase the patients, expectation on efficacy for pain, as it is well known that the analgesia induced placebo pills effects are associated with activity in the insula, cingulate, and thalamus, which are regions believed to be polarized by tDCS montages commonly used in pain trials [15].
A recent trial by Yoon et al. [16], which studied the brain metabolism changes after tDCS stimulation over the motor cortex in patients suffering from pain after SCI, showed a statistically significant decrease in pain ratings after the active tDCS.
A study by Soler et al. [17] suggested that the analgesic effect of tDCS differed according to the subtype of spontaneous pain, and those findings were confirmed by Fregni et al. trial.
The precise mechanism responsible for the active effects of the tDCS remain unknown, but it has been reported that tDCS over M1 induces activity changes in a number of brain regions, and that the unilateral M1 tDCS evokes significant activity changes in both the underlying M1 as well as M1 on the contralateral side of the brain. It is possible that those analgesic effects are possible through the tDCS influence on activity within regions such as the somatosensory thalamus.
In our study, we decided to refer to validated safety protocols [16] which included the use of relatively large wet sponges (25 cm2 to 35 cm2) and currents of 1 mA to 2 mA applied for duration of 20 min. For purpose of further studies, it might be useful to review those safety parameter in order to systematically elucidate the impact of the stimulation current settings, currently limited from safety purposes, on the analgesic outcomes looking, for example, at longer stimulation periods as well as thinking to use higher intensity and/or to apply it for longer interval of time each session, furthermore aspects related to electrode position and stimulation polarity could be revised. or it could be useful to review the stimulation protocols with regard to specific patient population.
The study by Yoon et al. [17] evaluated the underlying neural mechanisms of tDCS using [18] FDG-PET imaging, they found an increased metabolism in the medulla and decreased metabolism in the left dorsolateral prefrontal cortex (DLPFC) after active tDCS compared with sham tDCS. The left DLPFC changes were negatively correlated with pain relief. These results suggested that the analgesic effects of tDCS are associated with attentional modulation of pain perception through the DLPFC and medulla. Moreover, the increase in metabolism after active tDCS in the subgenual anterior cingulate cortex (sAAC) and insula suggest that tDCS modulates emotional components of the pain system.
The mechanism of tDCS is still not very well known, a work by Fritsch et al. [19] has shown that tDCS works on brain plasticity also by creating changes in the brain derived neurotrophic factor (BDNF) which has been associated with pain processing. In view of that we think that further studies looking at the relation between neurophysiology, biological markers and tDCS could be useful to improve our understanding on the tDCS effects on brain areas and furthermore for the optimisation the current stimulation protocols.
Our trial protocol overcame one of the Fregni et al. [11] study limitations since while in the before mentioned study subjects were allowed to change their medication regimen, we kept medications unchanged for all trial duration, which represented a challenge for the study.
Moreover, a study by Liebetanz et al. showed how antiepileptic medication and particularly carbamazepine interfere with the capability of motor cortex to react with sustained excitability changes to tDCS [20]. That is interesting to consider since, as mentioned, in our protocol we decided to continue the standard pain medications that the subjects were taking at the time of the trial. Since carbamazepine is one of the first line medication for neuropathic pain and the most of the subjects involved in our trial were on this treatment, we might hypothesize that a reduction in cortical effect after tDCS stimulation might be considered as a result of reduced excitability associated to long term neuroactive medication use in our population.
Another issue we faced has been linked to the hypothesis that the response to the tDCS stimulation could be variable in relation to the characteristic of the SCI lesion [12]. In facts, the links between pain and other variables such as level of injury, aetiology, completeness of SCI and psychosocial issues have not been extensively studied and an attempt at try to identify the SCI patients that show more improvements after the active treatment could be important to optimize future clinical trials. In our study we found clinical differences between the two groups which are related to the randomization, our sample population was randomized in a way that in the Sham group 6 participants out of 8 were complete SCI (AIS A), while in the Active group only 2 out of 7 were AIS A. Studies have suggested that variables such as advanced age at the time of injury, nature, onset intensity, bullet injury as a cause of trauma, early onset of pain in the weeks following the injury and associated symptoms (fatigue, infection, spasticity, constipation, urinary retention, joint pain, mood changes) are negative prognostic factors, whereas symptoms typically associated with neuropathic pain such as dysestesia, paroxysmal pain, location of SCI in thoracic and lumbar segments and sublesional pain are associated with positive response to brain stimulation, on the other hand completeness or incompleteness of the lesion has a neutral link with the response to the tDCS treatment [12].
Some strong points of our study protocol are that it has been designed and conducted in a double blinded manner and this is important since pain is a subjective variable and its evaluation as well as perception undergoes a significant placebo effect which is partially avoided with a double-blind trial method. Furthermore, it emerged that patient couldn’t guess if they received the active or the sham treatment, in fact no significant differences emerged when patients were questioned about that during the trial. This finding confirms that tDCS can be used efficaciously in double blinded studies.
After the brain stimulation, no one showed adverse effects, neither in the short term nor after the follow ups, therefore the safety of tDCS have been confirmed by our study.
Conclusion
In conclusion, it does appear to be a reduction in some pain measures particularly during the active phase (5 consecutive days of 20 mA tDCS stimulation), but comparisons between sham and active treatment group indicate that this could be a partial placebo type effect, as the group differences are not significant.
Our data show that in individuals with longstanding neuropathic SCI pain, tDCS focused over M1 does not provide pain relief, our results are similar to the study by Wringley et al. [2] and differ from the Fregni et al. study [11] which inspired our study design.
In conclusion, even if anodal tDCS is a non-invasive, low risk neuro stimulation technique to treat one of the most bothersome among the consequences of SCI, such as chronic pain is, we still need to prove its real efficacy and we are yet not ready to prescribe it as an active for chronic pain.
Acknowledgements
The authors thank Dr. Salman Lari for his assistance in conducting this trial.
References
- Widerström-NogaE G, Finnerup N B, Siddall PJ (2009) Biopsychosocial perspective on mechanisms-based approach to assessment and treatment of pain following spinal cord injury. J Rehabil Res Dev 46(1): 1-12.
- Wrigley PJ, Gustin SM, McIndoe LN, Chakiath RJ, Henderson LA (2013) Longstanding neuropathic pain after spinal cord injury is refractory to transcranial direct current stimulation: A randomized controlled trial. Pain 154(10): 2178-2184.
- Anke AGW, Stenheim AF, Stanghelle JK (1995) pain and life quality within 2 years of spinal cord injury. Paraplegia 33(10): 555-559.
- Felipe-Cuervo E, Yezierski RP (2001) Chronic pain after spinal injury: Interference with sleep and daily activities. Widerström-Noga EG1, Arch Phys Med Rehabil 82(11): 1571-1577
- Siddall PJ, Middleton JW (2006) Review: A proposed algorithm for the management of pain following spinal cord injury. Spinal Cord 44(2): 67-77
- Bonica’s Management of pain, fourth edition, Scott M. Fishmann. Press
- Hadjipavlou G, Cortese A M, RamaswamyB (2016) Bonica’s Management of pain, fourth edition, spinal cord injury and chronic pain. BJA Education 8: 1-5.
- Wallace BA, Ashkan K, Benabid AL (2004) Deep brain stimulation for the treatment of chronic, intractable pain. Neurosurg Clin N Am 15: 343-357.
- McDonald JW, Sadowsky C (2002) Spinal-cord injury. Seminar. Lancet 359: 417-425.
- Lang N, Siebner HR (2005) How does transcranial DC stimulation of the primary motor cortex alter regional neuronal activity in the human brain? Eur J Neurosci 22(2): 495-504.
- Fregni F, Boggio PS, Lima MC, Ferreira MJ, Wagner T, et al. (2006) A sham-controlled, phase II trial of transcranial direct current stimulation for the activeof central pain in traumatic spinal cord injury. Pain 122(12): 197-209.
- Moreno-Duarte I, Morse LR, Alam M, Bikson M, Zafonte R, et al. (2014) Target therapies using electrical and magnetic neural stimulation for the treatment of chronic pain in spinal cord injury. NeuroImage 1003-1013.
- Knotkova H, Nitsche MA, Cruciani RA (2013) Putative physiological mechanisms underlying tDCS analgesic effects. Frontiers in Human Neuroscience 7: 56-59.
- Nitsche MA, Cohen LG, Wassermann EM, Prioro A, Lang N, et al. (2008) Transcranial direct current stimulation: State of the art 2008, Brain Stimulation 1(3): 206-223.
- Schambra H, Bikson M, Wager T, DosSantos M, DaSilva A (2014) It’s all in your head: Reinforcing the placebo response with tDCS, Brain Stimul 7(4): 623-624.
- Bikson M, Datta A, Elwassif M (2009) Clin Neurophysiol. Establishing safety limits for transcranial direct current stimulation. Clinical Neuropsicol 120(6): 1033-1034.
- Yoon EJ, Kim YK, Kim HR, Kim SE, Lee Y, et al. (2014) Transcranial direct current stimulation to lessen neuropathic pain after spinal cord injury. A mechanistic pet study. Neurorehabil Neural Repair 28(3): 250-259.
- Soler MD, Kumru H, Pelayo R, Vidal J, Tormos JM, et al (2010) Effectiveness of transcranial direct current stimulation and visual illusion on neuropathic pain in spinal cord injury. Brain 2526-2577.
- Fritsch B, Reis J, Martinowich K, Schambra H, Ji Y, et al. (2010) Direct current stimulation promotes BDNF-dependent synaptic plasticity: potential implications for motor learning. Neuron 66(2): 198-204.
- Liebetanz D, Nitsche MA (2002) Pharmacological approach to the mechanisms of transcranial DC-stimulation-induced after-effects of human motor cortex excitability. Brain 125(Pt 10): 2238-2247.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences