Effect of Static Abdominals Training and Incentive Spirometer in Improvement of Pulmonary Function and Abdominal Strength in Spinal Cord Injury Patients- A Comparative Study
Mantri B, Pattnaik M and Mohanty P
DOI10.21767/2471-8173.100034
Mantri B, Pattnaik M and Mohanty P*
Swami Vivekanand National Institute of Rehabilitation Training and Research, Olatpur, Bairoi, Cuttack, India
- *Corresponding Author:
- Mohanty P
Swami Vivekanand National Institute
of Rehabilitation Training and Research
Olatpur, Bairoi, Cuttack, India
Tel: +919437487139
E-mail: ppmphysio@rediffmail.com
Received Date: March 24, 2017 Accepted Date: August 21, 2017 Published Date: August 27, 2017
Citation: Mantri B, Pattnaik M, Mohanty P (2017) Effect of Static Abdominals Training and Incentive Spirometer in Improvement of Pulmonary Function and Abdominal Strength in Spinal Cord Injury Patients- A Comparative Study. Spine Res Vol 3: No.2: 14 doi: 10.21767/2471-8173.100034
Abstract
Introduction: Following spinal cord injury, muscles below the level of injury develop variable degrees of disuse atrophy. Individuals with spinal cord injury (SCI) exhibit reduced lung volumes and flow rates as a result of respiratory muscle weakness. Many studies were done to strengthen diaphragm and abdominals using abdominal weights and dynamic curl up. Isolated training of abdominals using pressure biofeedback has been done by very few authors in patients with traumatic paraplegia.
Methodology: Traumatic paraplegics between T9-T12 were randomly selected. The selected subjects were randomly assigned in to static abdominals and incentive spirometry group. 15 subjects in each group. Subjects in first group receives static abdominal exercise using pressure biofeedback in crook lying while other group practiced expiratory muscle training using incentive spirometer. Both groups receive conventional physiotherapy exercises. Training was given for 5 days a week for 6 weeks.
Results: Result of the study suggested that both the static abdominals and incentive spirometry group had a significant improvement in pulmonary functions (FEV1, VC, MVV) and static abdominal strength in patients with traumatic paraplegia after treatment for 6 weeks. However, the incentive spirometry group showed greater change as compared to static abdominals.
Conclusion: Incentive spirometery training brings about more improvement in pulmonary function than static abdominals while static abdominals using pressure biofeedback leads to increase in strength of abdominal muscles compares to incentive spirometry.
Keywords
Spinal cord injury; Traumatic paraplegia; Spirometery training
Introduction
Spinal cord injury (SCI) is a low incidence high-cost disability requiring tremendous changes in an individual’s lifestyle. Spinal cord injuries may be traumatic or non-traumatic. Complete paralysis of all muscles involved with respiration occurs when the lesion is above C3; this type of injury requires immediate and ongoing ventilator support in order to sustain life. When the injury is between C3 and C5 (innervations of the diaphragm), respiratory insufficiency occurs via respiratory muscle dysfunction [1].
If thoracic segments are injured muscles of expiration is affected. Following spinal cord injury above T12, the impulses travelling down the cord to stimulate the abdominal muscles is interrupted. Associated factors such as decreased volume of air able to flow in and out of the lungs, also affect the ability to expel Sputum (or cough). The inability to effectively cough allows secretions, with trapped microbes, to remain in the lungs. This increases the risk of respiratory tract infections. Following spinal cord injury, muscles below the level of injury develop variable degrees of disuse atrophy. Muscle mass of all muscles innervated by spinal cord segment below the lesion decreased compared with control values. Mass of the external oblique, internal oblique and transverse abdominis muscles decreased significantly. Individuals with spinal cord injury (SCI) exhibit reduced lung volumes and flow rates as a result of respiratory muscle weakness [2].
Ventilation during exercise can be greatly compromised; the expiratory muscles actively contract in healthy people, whereas in SCI, partial or fully denervated expiratory muscles have impaired contractile activity and thus exhibit diminished exercise ventilation and ventilatory reserve. Although cough is an important defense mechanism against respiratory tract infections and atelectasis, the capacity to generate cough and clear respiratory secretions is severely compromised in most individuals with SCI due to the impaired innervations of the abdominal muscles at most SCI levels [1]. The contraction of the transverses abdominis is thought to contribute to dynamic stabilization of the lumbar spine [3].
It is often assumed that the prevalence of breathlessness due to specific task is greater at higher levels of SCI. Overall dyspnoea during activities of daily living is most common, among motorized wheel-chair users. In them dyspnoea noted while talking for more than a few minutes while hand-held propelled wheel-chair users more commonly experienced dyspnoea while dressing and undressing. In motorized wheelchair user, the relatively high rate of breathlessness during talking may be related to difficulty interrupting breathing to manipulate phrasing and speech loudness because their breathing is already greatly impaired. In fact, that patient with SCI activate their respiratory muscles in daily life less than able-bodied persons due to the lack of whole-body physical activity may also explain the weakened respiratory system. Therefore, special attention should be given to the functioning and improvement of their respiratory pump. Regular physical activity may be a decisive factor for the well-being of paraplegics and rehabilitation program improves the cardiorespiratory functioning. Loss of respiratory muscle strength, with ensuing ineffective cough and decreased ventilation, leads to pneumonia, atelectasis and respiratory insufficiency in sleep and while awake. These complications are generally preventable with careful serial assessment of respiratory function [2]. Kelley noted subjects with expiratory muscle weakness appear to have insufficient acceleration of the respiratory system at the onset of expiratory effort [4]. Dr. Sullivan C. recommended incentive spirometer (e.g. Tri-flow type) for home respiratory monitoring by patient [5]. Loh et al. suggested that incentive spirometer is cheap, easily available and reusable up to at least 50 times [6]. Rationale for Use of Isometric Exercise Loss of static muscle strength occurs rapidly with immobilization and disuse, with estimates from 8% per week to as much as 5% per day [7].
Many studies were done to strengthen diaphragm and abdominals using abdominal weights and dynamic curl up. Isolated training of abdominals using pressure biofeedback has been done by very few authors in patients with traumatic paraplegia.
Expiration is very much important for effective coughing. Expiratory training also decreases CO2 retention. Abdominal muscles are affected in paraplegics, and very less importance is given to them in rehabilitation and there is paucity of study on expiratory muscle training using pressure biofeedback. Therefore, the aim of our study was to compare the effect of incentive spirometry and static abdominals training in improving pulmonary function and static abdominals strength in patients with paraplegia.
Methodology
Design
Experimental design, comparison of two groups.
Sample size
30 (15 in each group)
Place of research
Neuro-rehab unit of department of physiotherapy, SVNIRTAR, Olatpur, Cuttack, Odisha.
Inclusion criteria
Traumatic paraplegics of lesion between T9-T12, age between 20 to 40 years, duration of onset 6 to 18 months, both male and female.
Exclusion criteria
Lesion above T9 and below T12, any other systemic disease of lungs. Eg. Asthma, pneumonia, cancer, patient with associated traumatic brain injury, subjects with orthopedic disorders (like rib fracture, PIVD etc), cardio-respiratory complication (like hypertension, pulmonary infections, preinjury history of pulmonary diseases or respiratory symptoms, Hypoxemia secondary to interruption of prescribed oxygen therapy etc).
Procedure
30 SCI subjects fulfilling the inclusion and exclusion criteria were randomly assigned into group 1- Static abdominals exercise using pressure biofeedback and group 2– Expiratory muscle training using incentive spirometry
After signing the consent forms. Detail assessment was done for all the subjects. Subjects were trained satisfactory with the programmed before beginning the study for few days, and then dependent variables were measured- Forced expiratory volume in 1 sec (FEV1), Vital capacity (VC), Maximum voluntary ventilation (MVV) by spirometry and static abdominal strength using pressure biofeedback.
Spirometry testing was performed by using the computerized spirometer (Minispir model, PC based USB spirometer). The persons with SCI were instructed to avoid consuming alcohol and caffeine 1 day before evaluation.
All the testing procedures was described and taught to the patient. Subjects carried out 3 FVC and 3 MVV tests while seated without any type of abdominal-binding support. All tests were carried out in accordance with American Thoracic Society guidelines for respiratory measurement.
Pressure biofeedback: The unit consists of a combined gauge and inflation bulb connected to a pressure cell. A simple device, designed by physical therapists, which registers changing pressure in an air-filled pressure cell allowing body movement, especially spinal movement, to be detected during exercise.
Group A: Patient position: Patient was made to lie in crook lying position.
Placement of instrument: The cushion was inflated to accommodate the existing space between the subject's lumbar spine and the exercise mat (approximately 40 mmHg).
Interventions: Subjects were given standard instructions to “Take a breath in and, as you exhale, gently draw your navel in toward your spine” to perform the ADIM. Then we asked the patient to maintain contraction for 10 seconds. Changes in pressure were recorded. The subject rested for 2 to 3 seconds after the 10 seconds maintenance. All the activities were performed in five sets of 10 repetitions each [8].
Group B: Subjects performed incentive spirometery (INS) for expiration. The INS group subjects were trained using an incentive spirometer; it is a flow oriented breathing exerciser. Subjects were asked to seat comfortably, hold spirometer at level and place mouthpiece in mouth. Breathing through mouth only, inhale and exhale through the spirometer. Nose clips were worn to ensure mouth breathing only. Then patients inhaled deeply, followed by forceful expiration. Patients were asked to maintain expiration for 10 seconds. Subjects of this group were instructed to keep the balls of the spirometer suspended for 10 seconds. This was repeated for 15 minutes daily for 5 days a week for a period of 6 weeks. If subjects felt fatigue or dizzy during exercise, rest was given for some time and then again exercises were performed [9].
Data collection
Measurements were taken prior to the beginning of treatment (0 week) and were repeated finally after the completion of treatment protocol (6th week).
Data analysis
Statistical analysis was performed using SPSS version 23.0
The dependent variables were analysed using repeated measures ANOVA. There was one between factor (group) with two levels (groups: Static abdominals and Incentive spirometry) and one within factor (time) with two levels (pretest and post-test). All pair wise post-hoc comparisons were analyzed using a 0.05 level of significance.
Results
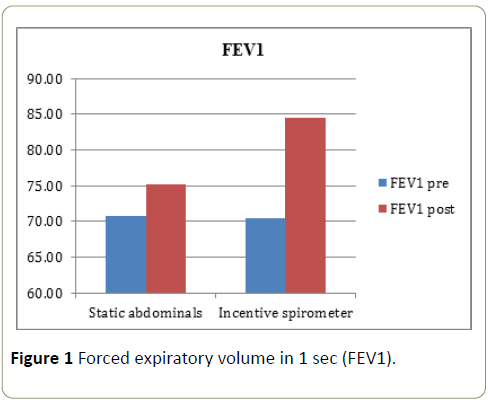
As depicted in Figure 1 there was a significant increase in FEV1 in both incentive spirometer and static abdominals group from pretreatment measurement to post treatment measurement over a period of 6 weeks. However Incentive spirometer group showed significant more improvement than static abdominals group.
There was main effect for time (1,28,0.05)=238.369, p=0.000. There was also a main effect for group (1,28,0.05)=9.759, p=0.004. The main effect was qualified into time X group interaction F (1,28,0.05)=66.702, p=0.000.
Post hoc analysis showed that the Incentive spirometer showed significantly greater increase in FEV1 when compared to Static abdominals group, from pre-to post test.
As depicted in Figure 2 there was a significant increase in VC in both incentive spirometer and static abdominals group from pretreatment measurement to post treatment measurement over a period of 6 weeks. However Incentive spirometer group showed significant more improvement than Static Abdominals group.
There was main effect for time (1,28,0.05)=163.023, p=0.000. There was also a main effect for group (1,28,0.05)=12.359, p=0.002. The main effect was qualified into time X group interaction F (1,28,0.05)=38.760, p=0.000
Post hoc analysis showed that the Incentive spirometer showed significantly greater increase in VC when compared to Static abdominals group, from pre-to post test.
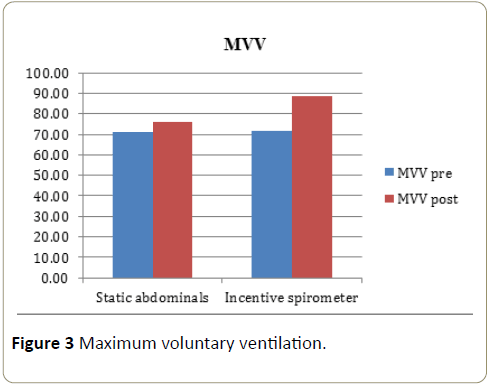
As depicted in Figure 3 there was a significant increase in MVV in both Incentive spirometer and Static Abdominals group from pretreatment measurement to post treatment measurement over a period of 6 weeks. However incentive spirometer group showed significant more improvement than static abdominals group.
There was main effect for time (1,28,0.05)=238.31, p=0.000. There was also a main effect for group (1,28,0.05)=9.609, p=0.004. The main effect was qualified into time X group interaction F (1,28,0.05) =68.618, p=0.000
Post hoc analysis showed that the Incentive spirometer showed significantly greater increase in MVV when compared to Static abdominals group, from pre-to post test.
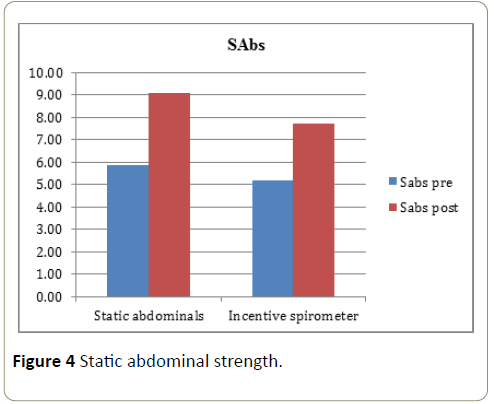
As depicted in Figure 4 there was a slight increase in static abs strength in both incentive spirometer and static abdominals group from pretreatment measurement to post treatment measurement over a period of 6 weeks. However, the value (P=0.289) is not statistically significant between the groups.
There was main effect for time (1,28,0.05)=240.254, p=0.000. There was also a main effect for group (1,28,0.05)=1.168, p=0.289. The main effect was qualified into time X group interaction F (1,28,0.05)=5.814, p=0.023
Discussion
The overall results of the study suggest that both static abdominals and incentive spirometry groups improved significantly from pre-to post treatment in all the four variables (FEV1, VC, MVV and static abdominal strength) at the end of six weeks. Incentive spirometry group showed significantly better improvement in FEV1, VC and MVV. However, the improvement shown in static abdominal strength was not statistically significant between the two groups.
FEV1 (Forced expiratory volume in 1 sec)
Results of this study shows there are marked increased in FEV1 value in both the groups. The mean improvement in FEV1 is 6.11% in static abdominals group while 19.95% in incentive spirometry group. Improvement is statistically significant within the group from pretreatment to post treatment. Improvement is statistically significant in incentive spirometry over static abdominals training.
Abdominal muscles are strong, and they play an important role in activities such as coughing and deep respiration. According to previous studies, deep abdominal muscles such as the TA and the multifidus muscle contribute not only to stabilization of the spine, and adjustment of posture, but also to significant improvements in pulmonary function, when ADIM was applied.
The advantages of using an incentive spirometer are: 1) it is easy to learn how to use the instrument; 2) it is economical; and 3) patients can be motivated to use it, as it produces a visible improvement. Its visual feedback helps to train patients to use the instrument independently and freely, and it maximizes their respiratory motivation.
Chang-Yong et al. studied short-term effects of respiratory muscle training combined with the abdominal drawing-in maneuvre on the decreased pulmonary function of individuals with chronic spinal cord injury. Similar results were found showing that the differences between the pre- and post-test values for FVC and FEV1 were significant among the groups. Post-test, in the ITG (integrated training group), the FVC and FEV1 values showed significant differences from those in the respiratory muscle training group (RMTG) and CG (control group). The increase in FEV1 following intervention may be due to the fact that the subjects became accustomed to RMT and ADIM and had their pulmonary functions measured repeatedly. However, the CG did not show a statistically significant difference, suggesting that there was no learning effect from repeated measurement and testing of pulmonary function [10].
Shehab et al. studied the effect of walking exercise and incentive spirometry in controlling age related respiratory muscle function changes in elderly. Both groups showed significant increases in VC, FEV1, PEF and PaO2. However, application of biofeedback assisted breathing exercises for patients with cystic fibrosis resulted in a significant improvement in VC, FEV1 and arterial oxygen saturation. These data suggest that respiratory muscle feedback assisted breathing exercise training may improve lung function in patients with cystic fibrosis [11].
In our study, we used biofeedback in both the groups by means of 3 balls used in incentive spirometry while change in pressure over cushion was provided by deflection over pressure cell.
Mi-Ra et al. used similar intervention to study the effects of the abdominal drawing-in maneuver and the abdominal expansion maneuvre (AEM) on grip strength, balance and pulmonary function in stroke patients. And found that the change of PEF (peak expiratory flow) in the ADIM (abdominal drawing-in maneuver) and AEM groups is larger compared with control group [12].
VC (Vital capacity)
Results of this study shows there are marked increased in VC value in both the groups. The mean improvement in VC is 8.89% in static abdominals group while 25.64% in incentive spirometry group. Improvement in values from pre-to post measurement was statistically significant within the group.
In our study VC is statistically significant in incentive spirometry over static abdominals training.
Various training programs like respiratory resistance or resistance endurance training, Inspiratory Muscle Strength Training (IMST), Abdominal Weights (AbWts) training with inspiratory muscle training, respiratory muscle training had been used to improve respiratory muscle strength, vital capacity and residual volume in spinal cord injury (SCI) patient [2].
Respiratory muscle training by incentive spirometer increases production of surfactant which leads to reducing surface tension, increasing lung compliance, decreasing the work of breathing and opening of collapsed alveoli to prevent atelectasis [13].
Our study utilized incentive spirometer and static abdominals as a therapeutic tool to improve respiratory muscle strength.
This is not surprising because the training was specifically directed toward improving expiratory pressure and, in fact, even used the same device to perform both training and measuring. This finding provides excellent evidence for the “specificity of training.” However, the following implications of this study’s findings are significant: simple expiratory muscle training performed by forced exhalation through a tube with resistance has the potential to increase expiratory muscle function in patients with acute spinal cord injury. By extrapolation, this training may have the potential to increase the strength and effectiveness of voluntary independent cough, decrease the amount of retained secretions, and thereby reduce the occurrence of pneumonias and other causes of respiratory morbidity. So “specificity of training” could be one of the reasons for improvement of strength and pulmonary functions in our study.
Walker et al. studied pulmonary function in quadriplegics. Pulmonary therapy consisted of incentive spirometry for 15 minutes a day 3 to 5 day per week. Resistance exercise consisted of pedaling an arm ergo meter up to 30 minutes three times a week. The mean vital capacity showing an average increase of 23.6%. The maximum volume of exhalation (max Ve) average increase is 69.6%. This improvement of VC in percentage are very close to our study, this may be because of we also used incentive spirometry for 5 days a week for 6 weeks [14].
In conclusion, expiratory muscle strength was significantly reduced and related to FVC, cough efficacy, and functional status. Expiratory muscle training tended to enhance inspiratory and expiratory muscle function. In addition, subjectively and objectively rated cough efficacy improved significantly and lasted for 3 months after training cessation.
MVV (Maximum voluntary ventilation)
Results of this study shows there are marked increased in MVV value in both the groups. The mean improvement in MVV is 7.11% in static abdominals group while 23.39% in incentive spirometry group. Improvement is statistically significant within the group from pretreatment to post treatment. Improvement is statistically significant in incentive spirometry over static abdominals training.
SCI lead to physical deconditioning which affect the different system of body and place less demand over the respiratory system for the physical activity so with prolong duration the respiratory muscles force as well endurance get reduced which may affect the MVV.
Activation of deep abdominal muscles, including the TA muscle, would be effective in enhancing respiratory capabilities. For patients with SCI who require intensive rehabilitation, ADIM helps these muscles to perform better during aerobic activities requiring endurance, thereby improving the performance of these patients in activities of daily living [10].
Sawant et al. studied effects of diaphragmatic weight training versus incentive spirometry in patients weaned from mechanical ventilation. They concluded that diaphragmatic weight training and incentive spirometry are effectual in improving pulmonary functions and dyspnoea. But when compared; improvement in MVV was better after training with incentive spirometry than diaphragmatic weight training [15].
Our result is also similar to their study showing significant improvement in MVV in incentive spirometer group.
Static abdominal strength (SAbs)
Results of this study shows there were marked increased in static abdominal strength in both the groups. The mean improvement in strength is 61.96% in static abdominals group while 48.65% in incentive spirometry group. Improvement in values from pre-to post measurement was statistically significant within the group.
Improvement is more in static abdominals group compare to incentive spirometry group, however improvement is not statistically significant in static abdominals over incentive spirometry training.
ADIM re-educates the respiratory muscles, improving muscle strength and endurance, as well as inducing powerful contraction of the respiratory muscles through repetitive afferent stimulation of the abdominal muscles. This increases intra-abdominal pressure, facilitating upward movement of the diaphragm, and decreases pleural pressure and lung volume, improving expiratory and sputum discharge abilities [10].
Static abdominals strength was improved more in ADIM training group compare to incentive spirometry. Simple ‘abdominal drawing-in’ would result in hypertrophy of TA and internal oblique [16]. It may be due to instrument adaptability because same instrument was used for training as well as measuring strength. According to “specificity of training” specific exercise elicits specific adaptations, creating specific training effects. The effects are most effectively induced by training the specific muscles energy systems involved.
Carolyn kisner, therapeutic exercise 5th edition
Isometric exercise is a static form of exercise in which a muscle contracts and produces force without an appreciable change in the length of the muscle and without visible joint motion. Although there is no mechanical work done (force × distance), a measurable amount of tension and force output are produced by the muscle. Based on the early research it was reported that isometric strength gains of 5% per week occurred when healthy subjects performed a single, nearmaximal isometric contraction everyday over a 6-week period. It helps to develop postural and joint stability [7].
Winser compares the effectiveness of abdominal weights (ABW) and incentive spirometry for improving the strength of diaphragm in tetraplegics. Comparison between the 2 groups showed statistically significant improvement in diaphragmatic strength among the ABW group. The mean EMG of diaphragm of ABW group raised from 1.1289 to 1.3036 mill volts with a significance of p<0.001, whereas it fell from 1.7001 to 1.0441 mill volts among INS group subjects with a significance of p<0.001. When comparing the EMG activities of both the groups a statistically significant improvement in diaphragmatic strength was observed among the ABW group [9].
EMST may have an improving effect on the activities of adjacent cortical areas. Following this concept, they concluded that certain processes of neuroplasticity in both the brain and spinal cord can occur as a result of the exercises per¬formed during EMST (17).
Conclusion
Incentive spirometer training brings about more improvement in pulmonary function than static abdominals while static abdominals using pressure biofeedback leads to increase in strength of abdominal muscles compares to incentive spirometry.
Limitations
Study sample was small, carry over effect was not being studied, there was no control group and recruitment of abdominal muscle was not studied using EMG.
Clinical Utility
Incentive spirometry can be used simultaneously in clinical as well as home based settings to improve pulmonary functions in patients with paraplegics.
The cost effectiveness and easy applicability seems to make incentive spirometry a useful adjunct to conventional physiotherapy.
Isolated control of abdomen as well as its strength can be improved by means of static abdominal exercise using pressure biofeedback.
References
- Sheel W (2008) Effects of exercise training and inspiratory muscle training in spinal cord injury: a systematic review. J Spinal Cord Med 31: 500-508.
- Bele A, Golhar S (2013) Utility of incentive spirometer and peak flow meter used as assessment as well as therapeutic tool to improve the respiratory muscle strength in wheelchair bound paraplegics in community. Online Int Interdisciplinary Res J 3: 44-62.
- Grooms D (2013) Clinimetric analysis of pressure biofeedback and transversus abdominis function in individuals with stabilization classification low back pain. Orthop J Sports Med 43:184-193.
- Kelley A (2003) Spirometry testing standards in spinal cord injury. Chest 123: 725-730.
- Sullivan C (2006) Home respiratory montoring of patient. The Lincolnshire Post-Polio Information Newsletter, Canada.
- Loh C, Ngor P, Rama S, Vijayasingham P, Thayaparan T (2005) Incentive spirometer as a means to score breathlessness. Malaysian J Med Sci 12: 39-50.
- Kisner C, Colby L (2017) Therapeutic exercise (5th edn). ISBN 0803615841.
- Kim CY, Lee JS, Kim HD, Kim IS (2015) Effects of the combination of respiratory muscle training and abdominal drawing-in maneuver on respiratory muscle activity in patients with post-stroke hemiplegia: A pilot randomization. Top Stroke Rehabil 22: 262-270.
- Winser S, George J, Stanley P, Tharion G (2009) A comparison study of two breathing exercise techniques in tetraplegics. Health 2: 88-92.
- Kim C, Lee J, Lee H (2017) Short-term effects of respiratory muscle training combined with abdominal drawing-in maneuver on decreased pulmonary function in people with chronic spinal cord injury: A pilot ran 40: 17-25.
- Shehab El-Kader MA (2013) Aerobic exercise training and incentive spirometry can control age-related respiratory muscles performance changes in elderly. Eur J Gen Med 10: 14-19.
- Yoon M, Choi H, Shin W (2015) Effects of the abdominal drawing-in maneuver and the abdominal expansion maneuver on grip strength, balance and pulmonary function in stroke patients. J Korean Physical Ther 27: 147-153.
- Kader S, Den Ashmawy E (2013) Aerobic exercise training and incentive spirometry can control age related pulmonary changes in elderly subjects. Eur J Gen Med 10: 14-19.
- Walker J, Cooney M, Norton S (1989) Improved pulmonary function in chronic quadriplegics after pulmonary therapy and arm ergometry 27: 278-283.
- Sawant A, Shinde N (2014) Effects of diaphragmatic weight training versus incentive spirometry in patients weaned from mechanical ventilation. A pilot study. Indian J Basic Appl Med Res 3: 24-30.
- Kulandaivelan S, Chaturvedi R (2014) Evidence based progressive core stabilization exercise formation for low core endurance individuals. Int J Physiother Res 2: 584-587.
- Laciuga H, Rosenbek JC, Davenport PW, Sapienza CM (2014) Functional outcomes associated with expiratory muscle strength training: Narrative review. J Rehabil Res Dev 51: 535-546.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences