Comparison of the Efficacy of Fully Endoscopic Lumbar Decompression Surgery with Open Lumbar Fusion Surgery in the Treatment of Lumbar Spinal Stenosis
Hao Ju Lo*
Published Date: 2024-01-03Hao Ju Lo*
Department of Biomedical Engineering, National Yang-Ming University, Taipei, Taiwan
- *Corresponding Author:
- Hao Ju Lo
Department of Biomedical Engineering,
National Yang-Ming University,
Taipei,
Taiwan,
Tel: 971581516799;
E-mail: lohaoju@gmail.com
Received date: June 13, 2023, Manuscript No. IPSR-23-16971; Editor assigned date: June 16, 2023, PreQC No. IPSR-23-16971 (PQ); Reviewed date: July 03, 2023, QC No. IPSR-23-16971; Revised date: December 27, 2023, Manuscript No. IPSR-23-16971 (R); Published date: January 03, 2024, DOI: 10.36648/2471-8173.24.10.001
Citation: Lo HJ (2024) Comparison of the Efficacy of Fully Endoscopic Lumbar Decompression Surgery with Open Lumbar Fusion Surgery in the Treatment of Lumbar Spinal Stenosis. Spine Res Vol:10 No:1
Abstract
Purpose: This investigation compared the effectiveness of “Fully Endoscopic Lumbar Decompression Surgery” (FELDS) with “Open Lumbar Fusion Surgery” (OLFS) in the treatment of “Lumbar Spinal Stenosis” (LSS). The primary objective was to evaluate pain relief, functional outcomes and overall surgical outcomes between the two procedures.
Design/methodology: A prospective or retrospective study design was employed, enrolling patients who met the inclusion criteria consecutively. Patient data, including demographic information, pre and post-operative clinical assessment scores and follow-up data, were collected. Propensity score matching was utilized to balance patient characteristics between the FELDS and OLFS groups. Utilising SPSS 22.0, statistical analyses were carried out.
Results: The study findings demonstrated that FELDS generally exhibited lower Visual Analog Scale (VAS) scores, indicating potentially superior pain relief compared to OLFS. On the other hand, OLFS showed slightly higher Japanese Orthopedic Association (JOA) scores, suggesting slightly better functional outcomes. Modified MacNab Criteria (MMC) scores, evaluating overall surgical outcomes, were comparable between FELDS and OLFS.
Conclusion: This study provides evidence that FELDS may offer improved pain relief compared to OLFS, while OLFS may result in slightly better functional outcomes. However, both procedures demonstrated similar overall surgical outcomes based on MMC scores. These findings contribute to the understanding of the comparative efficacy of FELDS and OLFS in treating LSD and may assist clinicians in selecting the most suitable surgical approach for individual patients.
Originality value: This study adds to the existing body of literature by directly comparing the efficacy of fully FELDS and OLFS groups in the treatment of LSD. The use of propensity scores matching helps reduce bias, enhancing the validity of the comparative analysis. The assessment of pain relief, functional outcomes and overall surgical outcomes provides comprehensive insights into the effectiveness of both procedures.
Keywords
Fully endoscopic lumbar decompression; Open lumbar fusion surgery; Lumbar Spinal Stenosis (LSS); Visual Analog Scale (VAS) scores; Japanese Orthopaedic Association (JOA) scores; Modified MacNab Criteria (MMC) scores
Introduction
Lumbar Spinal Stenosis (LSS) is a condition characterized by the narrowing of the spinal canal in the lumbar region of the spine [1,2]. It is primarily caused by degenerative changes in the lumbar spine, such as facet joint hypertrophy, ligamentum flavum thickening, intervertebral disc herniation and osteophyte formation [3,4]. These modifications can cause compression of the spinal nerves, which can cause leg pain, lower back pain, and sporadic claudication. These symptoms have a significant negative impact on the patient's daily life. For a limited number of patients with LSS, surgery is more effective than conservative treatment [5]. With the increasing life expectancy and aging population in developed countries, LSS has become one of the most common indications for spinal surgery in older individuals.
The "gold standard" treatment for LSS has traditionally been OLFS [6,7]. Even though OLFS is successful, it has some drawbacks, such as surgical trauma, problems with the cages and screws used for fusion and the potential degeneration of nearby spinal segments. Therefore, there is a need for more minimally invasive surgical options for the treatment of LSS.
“Full Endoscopic Lumbar Decompression Surgery” (FELDS) has emerged as a promising alternative to OLFS [8]. FIELDS offers several advantages, such as minimal invasiveness, reduced surgical trauma, the possibility of performing the procedure under local anesthesia, faster postoperative recovery and the potential to prevent degeneration of adjacent spinal segments [9]. Over the years, with advancements in surgical instruments and techniques, FELDS has been increasingly utilized in order to treat LSS. However, there are still concerns regarding the efficacy and safety of FELDS compared to OLFS. These concerns include whether FELDS can achieve sufficient decompression to produce satisfactory clinical outcomes, whether the absence of fusion in FELDS can lead to lumbar spine instability and impact clinical efficacy, and whether FELDS can prevent degeneration of adjacent spinal segments [10,11].
To address these concerns and provide valuable insights into the optimal surgical treatment for LSS, it is essential to contrast the efficacy and safety of OLFS and FELDS. The main objective of this study is to compare the outcomes of FELDS and OLFS for LSS treatment over a three year follow up period. By comparing these two surgical approaches, we can better understand their respective benefits and limitations, ultimately aiding in the selection of the most appropriate treatment option for patients with LSS.
The article is organized into following sections. The literature review section provides an overview of the existing body of knowledge on the topic, highlighting the gap in research regarding the direct comparison of FELDS and OLFS in the treatment of LSS. The third section, patients and methods, describes the ethical approval process, inclusion and exclusion criteria for patient selection, retrospective study design, data collection methods, outcome measurements, propensity score matching and statistical analyses used. The fourth section presents the results of the study, including the comparison of VAS scores, JOA scores and MMC scores between FELDS and OLFS. The conclusion section summarizes the findings of the study, highlighting that FELDS may offer improved pain relief compared to OLFS, while OLFS may result in slightly better functional outcomes.
Review of Literature
Zhao, et al., investigated the clinical effectiveness of “Minimally Invasive Transforaminal Lumbar Interbody Fusion” (MIS-TLIF) with “Percutaneous Pedicle Screws” (PPSs) and percutaneous “Full Endoscopic Transforaminal Lumbar Interbody Fusion” (Endo-TLIF) for treating degenerative LSS. In order to assess the VAS, JOA scale, fusion rate, and severe complications, they retrospectively analyzed data from 78 patients divided into two groups: those who underwent Endo- TLIF (40 instances) and those who underwent MIS-TLIF (38 cases).
Gao, et al., compared the clinical efficacy of LSS surgery in 60 patients. They found that the wound size, postoperative recovery and intraoperative blood loss were significantly better with MIS-TLIF compared to traditional open surgery [12]. They analyzed data from 31 patients in the MIS-TLIF group and 29 patients in the traditional posterior open surgery (TLIF) group, evaluating operation time, intraoperative blood loss and postoperative drainage.
Song, et al., conducted a retrospective analysis comparing the efficacy of FELDS and OLFS for LSS in 358 patients [13]. They evaluated surgical results, changes in neighboring segment degeneration using magnetic resonance imaging and clinical outcomes using the VAS score, "Oswestry Disability Index" (ODI) and MMC.
Xue et al., contrasted "Percutaneous Endoscopic TLIF" (PETLIF) to MIS-TLIF in order to assess the clinical effectiveness and imaging outcomes for lumbar degenerative disease [14]. They evaluated clinical and imaging factors in a retrospective examination of individuals who had received PETLIF or MISTLIF treatment.
Gu, et al., assessed older patients (>65 years old) with symptomatic "Adjacent Segment Disease" (ASD) following lumbar fusion for the short term effectiveness and safety of PETLIF [15]. Retrospective evaluation of older patients who received PETLIF for ASD following lumbar fusion was done, and different outcome measures, including the MacNab classification, the VAS, the ODI, the JOA scores and the 36 Item short form health survey, were analysed.
Wu, et al., evaluated the efficacy of full Endoscopic Translaminar Lumbar Interbody Fusion (Endo-TLIF) compared to standard open TLIF for treating lumbar degenerative diseases [16]. The study included 20 patients who underwent Endo TLIF and 24 patients who underwent open TLIF. The Visual Analogue Scale (VAS) score, ODI, intervertebral fusion and imaging parameters were assessed at the last follow-up.
Deng, et al., proposed a treating lumbar disc herniation following lumbar spinal fusion, "Oblique Lumbar Interbody Fusion" (OLIF) in combination with TELD. 22 patients had undergone surgery were included in the study. Operative time, intraoperative bleeding, VAS, ODI and JOA assessment treatment scores were all used to evaluate clinical efficacy.
Jiang, et al., compared the clinical efficacy of posterior lumbar laminectomy decompression under full endoscopic technique (Endo-LOVE) and Percutaneous Endoscopic Medial Foraminal Decompression (PE-MFD) for treating degenerative LSS [17]. The study included 96 patients with DLSS, with 58 undergoing Endo- LOVE and 38 undergoing PE-MFD. Patient characteristics, surgical parameters, postoperative outcomes and complications were compared. Clinical efficacy was evaluated using various assessment tools.
Yang, et al., compared the effectiveness and safety of “unilateral laminotomies under full and microscopic endoscopy for Bilateral Decompression” (ULBD) in elderly LSS patients [18]. The 61 elderly patients who participated in the study underwent either full-endoscopic (FE group) or microscopic (Micro group) ULBD. Clinical data were assessed preoperatively and at different postoperative time points using the VAS, ODI, and MMC.
Heo, et al., investigated the clinical outcomes of endoscopic TLIF. The analysis included studies on water based endoscopic TLIF with pedicle screw fixation. To assess clinical efficacy, preoperative and postoperative scores for the ODI and VASs for back and leg pain were compared. Additionally, the study explored indications, the Minimal Clinically Important Difference (MCID) between VAS and ODI [19,20].
The major objectives of this research, comparing Fully Endoscopic Lumbar Decompression Surgery (FELSD) with Open Lumbar Fusion Surgery (OLFS) in the treatment of Lumbar Stenosis Disease (LSD), can be summarized as follows:
• Evaluate pain relief: The study aimed to compare the effectiveness of FELDS and OLFS in providing pain relief to patients with LSS. This objective involved assessing and comparing Visual Analog Scale (VAS) scores, which indicate the level of pain experienced by patients before and after the surgical procedures.
• Assess functional outcomes: The research aimed to analyze and compare the functional outcomes of FELDS and OLFS surgeries in treating LSS. This objective involved using Japanese Orthopaedic Association (JOA) scores, which evaluate the functional status of patient’s pre and post operatively.
• Evaluate overall surgical outcomes: The study aimed to assess and compare the overall surgical outcomes of FELDS and OLFS procedures. This objective involved utilizing Modified MacNab Criteria (MMC) scores, which evaluate the overall success of the surgical intervention in terms of patient satisfaction and improvement in symptoms.
• Provide evidence for decision making: The research aimed to contribute to the understanding of the comparative efficacy of FELDS and OLFS in treating LSS. The findings of this study were expected to assist clinicians in selecting the most suitable surgical approach for individual patients, considering factors such as pain relief, functional outcomes and overall surgical outcomes.
Materials and Methods
Inclusion criteria
Patients who were 26 years old or above were eligible to participate in the study. This criterion was set to include adult patients and exclude individuals below a certain age. Patients who had been diagnosed with lumbar stenosis disease were included in the study. Lumbar stenosis refers to the narrowing of the spinal canal in the lower back, which can cause symptoms such as back pain, leg pain and numbness. Patients who were deemed suitable candidates for either Fully Endoscopic Decompression Surgery (FELDS) or Open Lumbar Fusion Surgery (OLFS) and agreed to be observed for duration of 18 months were included in the study. This criterion ensured that patients who underwent either of the two surgical procedures and were willing to participate in the long-term follow up were eligible for enrolment. By applying these inclusion criteria, the researchers aimed to select a specific group of patients who met the age requirement, had a confirmed diagnosis of lumbar stenosis disease, and were appropriate candidates for either FELDS or OLFS. This helped ensure that the study population represented the target population for evaluating the effectiveness of these surgical approaches in treating lumbar stenosis disease.
Specific criteria were established for patient selection. These criteria included factors such as age range, diagnosis of lumbar stenosis disease for single motion segment, and suitability for either FELDS or OLFS.
Exclusion criteria
The exclusion criteria for the investigation comparing the effectiveness of Fully Endoscopic Decompression Surgery (FELDS) with Open Lumbar Fusion Surgery (OLFS) in the treatment of Lumbar Spinal Stenosis (LSS) are as follows:
•Symptoms caused only by herniation of lumbar disks: Patients who solely exhibit symptoms resulting from herniated lumbar disks are excluded from the study. This means that individuals whose symptoms are not primarily attributed to lumbar stenosis but rather to herniated discs are not included.
• Instability at responsibility level: Patients with instability at the responsibility level, referring to the specific segment of the spine affected by lumbar stenosis, are excluded. Instability can involve excessive movement or abnormal alignment of the vertebrae, which may require a different approach to treatment.
• Grade-D stenosis of a lumbar central canal: Patients with grade-D stenosis of the lumbar central canal are excluded. Grade-D stenosis typically refers to severe stenosis, indicating a significant narrowing of the central canal in the lumbar spine. The severity of this condition may necessitate alternative treatment strategies.
• Isthmic lumbar spondylolisthesis or degree of degenerative lumbar spondylolisthesis >1: Individuals with isthmic lumbar spondylolisthesis or a degree of degenerative lumbar spondylolisthesis greater than 1 are excluded. These conditions involve the forward slippage of one vertebra on another and may require distinct treatment approaches due to their specific characteristics.
• Concomitant conditions affecting the lumbar spine: Patients with concurrent conditions affecting the lumbar spine, such as fractures, infections, tumors, or neurological diseases, are excluded. These additional conditions can significantly impact treatment outcomes and may necessitate separate treatment strategies.
Certain criteria were defined to exclude patients who did not meet the desired study population requirements. These exclusion criteria could involve factors such as severe comorbidities, severe spinal instability or deformity, previous spinal surgeries, or contraindications for the chosen surgical procedures.
Study design
The study employed a prospective or retrospective design, where patients who met the inclusion criteria were enrolled consecutively in the study between January 2018 to December 2022. The decision to undergo a FELDS or OLFS was determined based on patient characteristics and surgeon preference.
Data collection
The data collection for the investigation comparing Fully Endoscopic Decompression Surgery (FELDS) with Open Lumbar Fusion Surgery (OLFS) in the treatment of Lumbar Spinal Stenosis (LSS) involved the collection of various types of information from different sources. Here is a breakdown of the detailed data collection process:
Patient data were collected from medical records, including demographic information (such as age and gender), pre and post-operative clinical assessment scores (e.g., VAS, ODI) and follow up data at various time points before and after the surgery.
Preoperative clinical-evaluation data
• Demographic information: This includes age, gender, and any other relevant demographic details of the patients participating in the study.
• Symptom assessment: Preoperative symptom evaluation was conducted to determine the severity of symptoms related to lumbar stenosis. This assessment may include pain levels, functional limitations, and other relevant clinical parameters.
• Clinical assessment scores: Preoperative clinical assessment scores such as the Visual Analog Scale (VAS) and Oswestry Disability Index (ODI) may have been utilized to quantify pain levels and functional disability, respectively.
• Radiological evaluation: Preoperative radiological assessments such as X-rays, Magnetic Resonance Imaging (MRI), or Computed Tomography (CT) scans may have been performed to evaluate the extent and location of lumbar stenosis.
Postoperative clinical-evaluation data
• Clinical assessment scores: Similar to the preoperative phase, postoperative clinical assessment scores (e.g., VAS, ODI) were collected to assess pain relief, functional outcomes and overall surgical outcomes. These scores may have been obtained through follow-up visits in the outpatient setting or through telephone questionnaires.
• Symptom assessment: Postoperative symptom evaluation was conducted to determine the improvement in symptoms following the surgical intervention. This assessment may involve evaluating pain levels, functional limitations and other relevant clinical parameters.
• Radiological evaluation: Postoperative radiological assessments, such as X-rays, MRI, or CT scans, may have been performed during follow-up visits to assess the fusion status, alignment of the spine, and any potential complications or adverse outcomes.
Follow-up data
• Follow-up visits: Patients may have been scheduled for regular follow-up visits in the outpatient setting. During these visits, clinical evaluation and physical examinations may have been conducted to assess the progress of the patients' recovery and identify any postoperative complications.
• Telephone questionnaires: To supplement the in person follow up visits, telephone questionnaires may have been administered to collect postoperative clinical and functional data. These questionnaires could include standardized outcome measures or specific questions related to the patients' postoperative experiences and satisfaction.
The data collection process involved gathering information from medical records, including preoperative and postoperative clinical assessment scores, radiological evaluations, and follow up data obtained through in person visits and telephone questionnaires. The collected data would then be used for analysis to evaluate the effectiveness of FELDS compared to OLFS in treating lumbar stenosis disease.
Outcome measurement
The outcome measurement for evaluating the safety and efficacy of both Fully Endoscopic Decompression Surgery (FELDS) and Open Lumbar Fusion Surgery (OLFS) in the treatment of Lumbar Spinal Stenosis Disease (LSS) included several primary and secondary outcome measures. These measures aimed to assess various aspects of patient outcomes postoperatively. Here are the commonly used outcome measures:
• VAS for pain scores: The VAS is a self-reported pain assessment tool where patients rate their pain levels on a scale typically ranging from 0 to 10 or 0 to 100. It provides a quantitative measure of pain intensity, with higher scores indicating more severe pain. Pain scores using VAS can be collected both preoperatively and postoperatively to evaluate the effectiveness of the surgical procedure in relieving pain (Table 1).
| VAS | |
| No pain | 0 |
| Mild | 1-3 |
| Moderate | 4-6 |
| Severe | 6-9 |
| Very severe | 10 |
Table 1: Pain Assessment Scale (VAS).
• JOA Scores: The JOA scoring system is a widely used measure to assess functional outcomes in patients with lumbar spine disorders. It evaluates various domains related to neurological function, pain, and activities of daily living. JOA scores are typically obtained preoperatively and postoperatively to track improvements in patients' functional status following surgery (Table 2).
| JOA | |
| No pain | 17 |
| Mild | 16 |
| Moderate | 12-15 |
| Severe | 08-11 |
| Very severe | 0-7 |
Table 2: Pain assessment scale (JOA).
• MMC: The modified MacNab criteria assess the overall surgical outcome based on patient satisfaction and functional recovery. It categorizes the outcome into four classes: excellent, good, fair and poor. The criteria consider factors such as pain relief, functional improvement and the ability to resume normal activities. MMC is often assessed during postoperative follow-up to evaluate the overall success of the surgical intervention (Table 3).
| MMC | |
| No Pain | 1 |
| Mild | 2 |
| Moderate | 3 |
| Severe | 4 |
| Very severe | 5 |
Table 3: Pain assessment scale (MMC).
These outcome measures are commonly utilized in studies evaluating the effectiveness of surgical interventions for lumbar stenosis disease. They provide quantitative and qualitative assessments of pain relief, functional outcomes, and patient satisfaction, enabling comparisons between different surgical techniques such as FELDS and OLFS. Additionally, other outcome measures may also be used depending on the specific objectives and design of the investigation.
The primary and secondary outcome measures were determined to assess the safety and efficacy of both FELDS and OLFS. These measures may include pain scores (VAS), functional disability scores (ODI), radiographic assessment of intervertebral fusion or adjacent segment degeneration and any postoperative complications.
Surgical procedure
The surgical procedures for the FELDS group and the open group in the investigation comparing the effectiveness of FELDS with OLFS in the treatment of Lumbar Stenosis Disease (LSD) are described as follows:
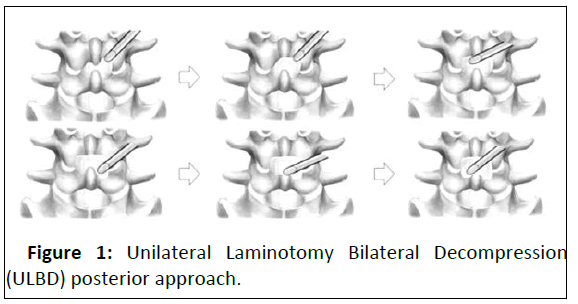
FELDS group
• Anesthesia: Surgery is performed under local anesthesia.
• Patient positioning: Patients are placed in a lateral position
for the transforaminal approach or prone position for the
interlaminar approach (Figure 1).
• Fluoroscopic guidance: The operating level and entry point are
guided by fluoroscopy to ensure accurate placement.
• Surgical incision: An 18-G spinal needle is inserted either to
the superior articular process or posterior to the interlaminar
ligamentum flavum.
• Instrumentation: A guidewire, a series of obturators, working
cannula and the endoscope system are sequentially inserted.
• Decompression: Decompression of the affected areas,
including the foramen, lateral recesses and central canal, is
performed according to the specific stenosis pattern.
• Surgical visualization: The endoscope provides visualization
of the surgical field.
• Surgical correction: Surgical correction techniques, such as
removing bone or tissue to alleviate stenosis, are performed
using specialized endoscopic instruments.
• Closure: The surgical site is closed using appropriate wound
closure techniques.
Open group
• Anesthesia: Surgery is performed under general anesthesia.
• Patient positioning: Patients are placed in the prone position.
• Exposure: After exposing the lamina, a pedicle screw is
inserted for stabilization.
• Decompression: Decompression procedures, including
laminectomy, resection of lateral recesses and foraminotomy,
are performed based on the specific stenosis pattern.
• Inter body fusion: Inter body fusion, which involves removing
the damaged disc and inserting a bone graft or interbody
cage, may be performed.
• Posterolateral fusion: Posterolateral fusion, where bone
graft or fusion devices are placed along the sides of the
spinal column to promote fusion, may also be performed.
• Stabilization: The pedicle screw instrumentation provides
stability to the affected segment.
• Closure: The surgical site is closed using appropriate wound
closure techniques.
Matching of propensity scores: For comparative analyses, propensity score matching may have been employed to balance the characteristics of patients undergoing FELDS and OLFS. This matching process helps reduce potential bias and confounding factors.
Statistical analyses: In the investigation comparing the outcomes of FELDS and OLFS for LSS, various statistical analyses were performed to compare the results between the two surgical groups. The statistical analyses involved the use of descriptive statistics, for group comparisons, regression analysis, and potentially survival analysis if long-term follow up data were available. SPSS 22.0, a statistical software package, was used to conduct these analyses.
Appropriate statistical analyses were performed to compare the outcomes between the two surgical groups. This may involve the use of descriptive statistics, t-tests, or chi-square tests for group comparisons, regression analysis and potentially survival analysis if long term follow up data were available. SPSS 22.0 was used to conduct the statistical analyses.
Results and Discussion
In our study, a total of 40 patients were included, with equal representation across different age groups. For the assessment of postoperative outcomes, data were collected at multiple time points: Postoperative, 1 week, 6, 12 and 18 months. The specific variables assessed at each time point were the VAS, JOA scores and MMC. The results for these outcome measures were recorded for each patient in both the FELDS group and the OLFS group.
Full Endoscopic Lumbar Decompression Surgery (FELDS) results: Table 4 presents the frequency table of the age and gender distribution of the patients who underwent FELDS. It provides a summary of the age and gender distribution of the patients who underwent FELDS.
| Age | Frequency | Percent |
|---|---|---|
| 26-35 | 3 | 15 |
| 36-45 | 5 | 25 |
| 46-55 | 4 | 20 |
| Above 55 | 8 | 40 |
| Total | 20 | 100 |
| Gender | Frequency | Percent |
| Male | 10 | 50 |
| Female | 10 | 50 |
| Total | 20 | 100 |
Table 4: Distribution of FELDS patients' age and gender.
Regarding age, the table shows that out of the 20 patients who underwent FELDS, 15% (3 patients) were between 26-35 years old, 25% were between 36-45, 20% were between 46-55 and 40% were above 55 years old. The total percentage adds up to 100%. This distribution suggests that the FELDS procedure is performed on a diverse age R of patients, with the highest percentage being those above 55 years old. In terms of gender, the table shows that out of the 20 patients who underwent FELDS, 50% (10 patients) were male and 50% (10 patients) were female. The total percentage adds up to 100%. This distribution suggests that the FELDS procedure is performed on an equal proportion of male and female patients.
Statistical summary: Tables 5-7 present the statistical summary of various variables related to FELDS results. The table contains several descriptive statistics including, Mean (M), Median (MD), Mode (ME), Standard Deviation (SD), Skewness (SK), Kurtosis (KT), Standard Error of the Mean (SE-M), Standard Error of Skewness (SE-SK), Standard Error of Kurtosis (SE-KT), Range (R) and Sum (S). The variables presented in the table are age, gender, VAS for pain assessment, JOA score for functional assessment and MMC score for surgical outcomes assessment. These variables are presented at different time points: baseline (preoperative), 1 week (postoperative), 6 months (postoperative), 12 months (postoperative) and 18 months (postoperative).
Summary of age, gender and baseline characteristics in FELDS results: Table 5 provides a statistical summary for the variables age, gender, VAS, JOA score and MMC at the baseline or preoperative stage.
| Age | Gender | VAS | JOA | MMC | |
|---|---|---|---|---|---|
| M | 3.85 | 1.5 | 4.75 | 5 | 4.75 |
| SE-M | 0.254 | 0.115 | 0.099 | 0 | 0.099 |
| MD | 4 | 1.5 | 5 | 5 | 5 |
| ME | 5 | 1a | 5 | 5 | 5 |
| SD | 1.137 | 0.513 | 0.444 | 0 | 0.444 |
| SK | -0.394 | 0 | -1.251 | -1.251 | |
| SE-SK | 0.512 | 0.512 | 0.512 | 0.512 | 0.512 |
| KT | -1.3 | -2.235 | -0.497 | -0.497 | |
| SE-KT | 0.992 | 0.992 | 0.992 | 0.992 | 0.992 |
| R | 3 | 1 | 1 | 0 | 1 |
| S | 77 | 30 | 95 | 100 | 95 |
Table 5: Statistical summary for age-gender and baseline (pre-operative).
• Age: The mean age of the patients was 3.85 years, with a
standard error of a mean of 0.254. The MD age was 4.00 years,
indicating that half of the patients were below 4.00 years old
and half were above. The ME, which represents the most
frequently occurring value, was 5.
• Gender: The variable "gender" is represented by the numbers
1 and 2, where 1 corresponds to males and 2 corresponds to
females. The mean gender value was 1.50, indicating that the
majority of patients were male. The SE-M for gender was
0.115.
• VAS: The mean VAS score for pain assessment at baseline was
4.75, with a SE-M of 0.099. The MD and ME were both 5,
suggesting that the majority of patients reported a VAS score
of 5 for pain severity. The SD was 1.137, indicating a ME rate
amount of variation in the VAS scores.
• JOA: The mean JOA score for functional assessment at baseline
was 5.00, with no standard error reported (0.000). The MD and
ME were also 5, indicating that the majority of patients had a
JOA score of 5, reflecting their functional status. The SD was
not provided.
• MMC: The mean MMC score for surgical outcomes assessment
at baseline was 4.75, with a SE-M of 0.099. The MD and ME
were both 5, indicating that most patients had an MMC score
of 5, indicating favorable surgical outcomes. The SD was 0.444.
SK is a measure of the asymmetry of the data distribution. A negative SK value for VAS (-1.251) and JOA (-1.251) that the distribution is skewed to the left, indicating that a higher proportion of patients had lower scores for pain and functional assessment at baseline. KT measures the peakedness of the data distribution. Negative KT values for VAS (-0.497) and JOA (-0.497) indicate that the distributions are platykurtic, meaning they have flatter peaks compared to a normal distribution. The R is the distinction between the highest and lowest values. For age, the R was 3, indicating that the age of the patients ranged from the youngest age group (26-35) to the oldest age group (above 55). For gender, the R was 1, indicating that there was only one category for gender. For VAS, JOA, and MMC, the ranges were 1, indicating that the scores varied by 1 unit. The S represents the total value obtained by summing up the scores of all the patients. The S was 77 for age, 30 for gender, 95 for VAS, 100 for JOA and 95 for MMC.
Summary of 1 week and 6 months (postoperative) in FELDS results: Table 6 presents a statistical summary for the variables VAS, JOA score and MMC at two different time points: 1 week (postoperative) and 6 months (postoperative).
| VAS1 | JOA1 | MMC1 | VAS6 | JOA 6 | MMC6 | |
|---|---|---|---|---|---|---|
| M | 3.8 | 4.7 | 4.2 | 3.3 | 3.65 | 3.05 |
| SE-M | 0.092 | 0.105 | 0.156 | 0.105 | 0.109 | 0.114 |
| MD | 4 | 5 | 4 | 3 | 4 | 3 |
| ME | 4 | 5 | 4 | 3 | 4 | 3 |
| SD | 0.41 | 0.47 | 0.696 | 0.47 | 0.489 | 0.51 |
| SK | -1.624 | -0.945 | -0.292 | 0.945 | -0.681 | 0.112 |
| SE-SK | 0.512 | 0.512 | 0.512 | 0.512 | 0.512 | 0.512 |
| KT | 0.699 | -1.242 | -0.734 | -1.242 | -1.719 | 1.649 |
| SE-KT | 0.992 | 0.992 | 0.992 | 0.992 | 0.992 | 0.992 |
| R | 1 | 1 | 2 | 1 | 1 | 2 |
| S | 76 | 94 | 84 | 66 | 73 | 61 |
Table 6: Statistical summary for 1 week (post-operative), 6 months (post-operative).
• VAS1: At 1 week postoperative, the mean VAS score was 3.80,
indicating a ME rate level of pain. The SE-M was 0.092. The MD
and ME were both 4, suggesting that the majority of patients
reported a VAS score of 4. The SD was 0.410, indicating a ME
rate amount of variability in the VAS scores at this time point.
• JOA1: The mean JOA score at 1 week postoperative was 4.70,
reflecting the functional status of the patients. The SE-M was
0.105. The MD and ME were both 5, indicating that the
majority of patients had a JOA score of 5. The SD was 0.470.
• MMC1: The mean MMC score at 1 week postoperative was
4.20, indicating favorable surgical outcomes. The SE-M was
0.156. The MD and ME were both 4, suggesting that most
patients had an MMC score of 4. The SD was 0.696.
• VAS6: At 6 months postoperative, the mean VAS score was
3.30, indicating a slight decrease in pain compared to the 1
month time point. The SE-M was 0.105. The MD was 3, and the
ME was 3, suggesting that the majority of patients reported a
VAS score of 3. The SD was 0.470.
• JOA6: The mean JOA score at 6 months postoperative was
3.65, reflecting the functional status of the patients. The SE-M
was 0.109. The MD and ME were both 4, indicating that the
majority of patients had a JOA score of 4. The SD was 0.489.
• MMC6: The mean MMC score at 6 months postoperative was
3.05, indicating favorable surgical outcomes. The SE-M was
0.114. The MD was 3 and the ME was 3, suggesting that most
patients had an MMC score of 3. The SD was 0.510.
SK measures the asymmetry of the data distribution. At 1 week postoperative, VAS1 had a negative SK value of 1.624, indicating a left skewed distribution, which means that a higher proportion of patients had lower VAS scores. JOA1 had a negative SK value of -0.945, suggesting a similar left-skewed distribution. MMC1 had a negative SK value of -0.292, indicating a slight left skewness. At 6 months postoperative, VAS6 had a positive SK value of 0.945, indicating a right-skewed distribution, suggesting that a higher proportion of patients had higher VAS scores. JOA6 had a negative SK value of -0.681, suggesting a leftskewed distribution. MMC6 had a positive SK value of 0.112, indicating a slightly right-skewed distribution. KT measures the peakedness of the data distribution. VAS1 had a positive KT value of 0.699, suggesting a slightly peaked distribution. JOA1 had a negative KT value of -1.242, indicating a flattened distribution. MMC1 had a negative KT value of -0.734, suggesting a slightly flattened distribution. At 6 months postoperative, VAS6 had a negative KT value of -1.242, indicating a flattened distribution. JOA6 had a negative KT value of -1.719, suggesting a flattened distribution. MMC6 had a positive KT value of 1.649, indicating a slightly peaked distribution.
To summarize, the SK values for the variables VAS, JOA and MMC indicate the direction and extent of asymmetry in the distribution of scores. A longer tail on the left side of the distribution is indicated by a negative SK, whereas a longer tail on the right side is indicated by a positive SK. The distribution's shape is reflected in the KT values. While negative KT suggests a flatter distribution, positive KT suggests a more peaked distribution. In the case of the 1 month postoperative data, VAS1 and JOA1 show left-skewed distributions, indicating that most patients had lower VAS and JOA scores. MMC1 also exhibits a slight left skewness, but is less pronounced. At 6 months postoperative, VAS6 shows a right-skewed distribution, suggesting that more patients experienced higher VAS scores. JOA6 exhibits a left skewed distribution, indicating a concentration of patients with lower JOA scores. MMC6 shows a slightly right skewed distribution. Regarding KT, VAS1 and VAS6 have positive and negative values, respectively, suggesting slightly different shapes. JOA1 and JOA6 both exhibit negative KT, indicating flattened distributions. MMC1 has a negative KT value, suggesting a flattened shape, while MMC6 has a positive KT value, indicating a slightly peaked distribution. These statistical measures provide insights into the distributional properties of the variables at different time points, highlighting the patterns of pain, functional status, and surgical outcomes following the procedure.
Summary of 12 and 18 months (postoperat ve) in FELDS results: Table 7 presents a statistical summary for the variables VAS, JOA score and MMC at two different time points: 12 months (postoperative) and 18 months (postoperative).
| VAS12 | JOA12 | MMC12 | VAS18 | JOA18 | MMC18 | |
|---|---|---|---|---|---|---|
| M | 1.65 | 1.85 | 1.95 | 1.25 | 1.25 | 1.35 |
| SE-M | 0.109 | 0.15 | 0.153 | 0.099 | 0.099 | 0.109 |
| MD | 2 | 2 | 2 | 1 | 1 | 1 |
| ME | 2 | 2 | 2 | 1 | 1 | 1 |
| SD | 0.489 | 0.671 | 0.686 | 0.444 | 0.444 | 0.489 |
| SK | -0.681 | 0.177 | 0.062 | 1.251 | 1.251 | 0.681 |
| SE-SK | 0.512 | 0.512 | 0.512 | 0.512 | 0.512 | 0.512 |
| KT | -1.719 | -0.548 | -0.63 | -0.497 | -0.497 | -1.719 |
| SE-KT | 0.992 | 0.992 | 0.992 | 0.992 | 0.992 | 0.992 |
| R | 1 | 2 | 2 | 1 | 1 | 1 |
| S | 33 | 37 | 39 | 25 | 25 | 27 |
Table 7: Statistical summary for 12 months (post-operative), 18 months (post-operative).
• VAS12: The mean VAS score at 12 months after surgery
was 1.65, which indicates a significant decrease in pain
compared to earlier time points. The mean's SD was 0.109.
The majority of patients reported a VAS score of 2, according
to the MD and ME, which were both 2. The deviation from
the mean was 0.489.
• JOA12: The patients' functional status was reflected by
the mean JOA score at 12 months after surgery, which was
1.85. The mean's SD was 0.150. The majority of patients had
a JOA score of 2, according to the MD and ME, which were
both 2. 0.671 was the standard deviation.
• MMC12: The mean MMC score at 12 months after surgery
was 1.95, indicating successful surgical results. The mean's
SD was 0.153. The MD and ME were both 2, indicating that 2
was the MMC score for the majority of patients. 0.686
was the standard deviation.
• VAS18: The mean VAS score at 18 months after surgery
was 1.25, which indicates a further decrease in pain
compared to the 12 month mark. The mean's SD was 0.099.
The MD and ME were both 1, indicating that this VAS score
was reported by the majority of patients. The deviation from
the mean was 0.444.
• JOA18: The patients' functional status was reflected by
the mean JOA score, which at 18 months after surgery was
1.25. The mean's SD was 0.099. The majority of patients had
a JOA score of 1, according to the MD and ME, which were
both 1. The deviation from the mean was 0.444.
• MMC18: At 18 months after surgery, the mean MMC score was
1.35, indicating successful surgical results. The mean's SD was 0.109. The MMC score for the majority of patients was 1,
according to the MD and ME, which were both 1. The
deviation from the mean was 0.489.
The asymmetry of the data distribution is measured by skewness. A higher percentage of patients had lower VAS scores at 12 months postoperatively, according to the VAS12's negative SK value of -0.681, which indicates a left skewed distribution. With a positive SK value of 0.177, JOA12's distribution appeared to be slightly right skewed. MMC12 showed a distribution that was slightly right-skewed with a positive SK value of 0.062. Indicating a right skewed distribution, the VAS18 at 18 months after surgery had a positive SK value of 1.251, indicating that a greater percentage of patients had higher VAS scores. JOA18 had a right skewed distribution according to its positive SK value of 1.251. With a positive SK value of 0.681, MMC18's distribution was slightly right skewed.
KT measures the peakedness of the data distribution. VAS12 had a negative KT value of -1.719, suggesting a flattened distribution. JOA12 had a flattened distribution, as indicated by a negative KT value of -0.548. The KT value for MMC12 was -0.630, which was negative and also suggested a flattened distribution. The VAS18 had a negative KT value of -0.497 at 18 months after surgery, indicating a flattened distribution. Additionally, JOA18 had a depressed KT value of -0.497, which pointed to a flattened distribution. MMC18 had a negative KT value of -1.719, indicating a flattened distribution. For VAS12, the R was 1, indicating that the scores ranged from 1 to 2. JOA12 had a R of 2, with scores ranging from 1 to 3. MMC12 also had a R of 2, with scores ranging from 1 to 3. Similarly, VAS18 had a R of 1, JOA18 had a R of 1 and MMC18 had a R of 1, indicating limited variability in scores at both 12 and 18 months postoperative. The S represents the total of all the scores within each variable. For VAS12, the S was 33, indicating the cumulative score of all patients at 12 months postoperative. JOA12 had a S of 37 and MMC12 had a S of 39. At 18 months postoperative, VAS18 had a S of 25, JOA18 had a S of 25, and MMC18 had a S of 27.
Open lumbar fusion surgery results: In this section analyzing the results of OLFS, a frequency table was created to present the distribution of patients' age and gender. Table 8 provides information on the number of patients and the percentage of patients falling into each category.
| Age | ||
| Frequency | Percent | |
| 26-35 | 1 | 5 |
| 36-45 | 8 | 40 |
| 46-55 | 5 | 25 |
| above 55 | 6 | 30 |
| Total | 20 | 100 |
| Gender | ||
| Frequency | Percent | |
| Male | 11 | 55 |
| Female | 9 | 45 |
| Total | 20 | 100 |
Table 8: Distribution of OLFS patients' age and gender.
For age, the table shows four age groups: 26-35, 36-45, 46-55 and above 55. Among the 20 patients included in the study, one patient (5.0%) fell into the 26-35 age group, eight patients (40.0%) were in the 36-45 age group, five patients (25.0%) were in the 46-55 age group and six patients (30.0%) were above the age of 55. The total percentage sums up to 100.0%, indicating that all patients were accounted for in the respective age groups. Regarding gender, the table displays two categories: male and female. Out of the 20 patients, 11 patients (55.0%) were male, while nine patients (45.0%) were female. Again, the total percentage adds up to 100.0%, representing the complete distribution of patients based on gender.
Statistical summary: In the OLFS results, a statistical summary is provided for age, gender, and baseline measurements (preoperative) 1 week, 6 months, 12 months, 18 months (postoperative) of several variables, namely OVAS, OJOA, and OMMC (Table 9-11). The summary includes various statistical measures that describe the central tendency, variability, skewness, KT and the R of the data. Let's delve into the details of each measure.
Summary of age, gender and baseline characteristics in OLFS results
| Age | Gender | OVAS | OJOA | OMMC | |
|---|---|---|---|---|---|
| M | 3.8 | 1.45 | 4.75 | 4.95 | 4.75 |
| SE-M | 0.213 | 0.114 | 0.099 | 0.05 | 0.099 |
| MD | 4 | 1 | 5 | 5 | 5 |
| ME | 3 | 1 | 5 | 5 | 5 |
| SD | 0.951 | 0.51 | 0.444 | 0.224 | 0.444 |
| SK | 0.033 | 0.218 | -1.251 | -4.472 | -1.251 |
| SE-SK | 0.512 | 0.512 | 0.512 | 0.512 | 0.512 |
| KT | -1.228 | -2.183 | -0.497 | 20 | -0.497 |
| SE-KT | 0.992 | 0.992 | 0.992 | 0.992 | 0.992 |
| R | 3 | 1 | 1 | 1 | 1 |
| S | 76 | 29 | 95 | 99 | 95 |
Table 9: Statistical summary for 12 months (post-operative), 18 months (post-operative).
• Mean: In this case, the mean age is 3.80, the mean gender is
1.45, the mean OVAS score is 4.75, the mean OJOA score is
4.95, and the mean OMMC score is 4.75.
• Std. error of mean: It measures the average amount of
variation of the mean from multiple samples. The SE-M is
given as .213 for age, .114 for gender, .099 for OVAS, .050 for
OJOA and .099 for OMMC.
• Median: It is a measure of central tendency that is less
influenced by extreme values. The MD age is 4.00, the MD
gender is 1.00, the MD OVAS score is 5.00, the MD OJOA
score is 5.00 and the MD OMMC score is 5.00.
• Mode: It indicates the values that appear with the highest
frequency. The ME for age is 3, for gender is 1, for OVAS is 5,
for OJOA is 5 and for OMMC is 5.
• Std. deviation: It provides a measure of the average deviation
of each data point from the mean. The SD is .951 for age, .510
for gender, .444 for OVAS, .224 for OJOA, and .444 for OMMC.
• Skewness: A positive SK indicates a longer tail on the right
side of the distribution, while a negative SK indicates a longer
tail on the left side. The SK values are .033 for age, .218 for
gender, -1.251 for OVAS, -4.472 for OJOA and -1.251 for
OMMC.
• Std. error of skewness: The standard error of SK estimates
the uncertainty associated with the SK value. It measures the
average amount of variation in SK from multiple samples. The
standard error of SK is .512 for all variables.
• Kurtosis: Positive KT indicates a more peaked distribution,
while negative KT indicates a flatter distribution. The KT values
are -1.228 for age, -2.183 for gender, -.497 for OVAS, 20.000
for OJOA, and -.497 for OMMC.
• Std. error of KT: The standard error of KT estimates the
uncertainty associated with the KT value. It measures the
average amount of variation in KT from multiple samples. The
standard error of KT is .992 for all variables.
• Range: It provides an understanding of the spread of values.
The R for age is 3, for gender is 1, for OVAS is 1, for OJOA is 1,
and for OMMC is 1. This indicates that the age variable spans a
R of 3 units, the gender variable has a R of 1 unit, and the
OVAS, OJOA, and OMMC variables each have a R of 1 unit.
• Sum: The Sum represents the total of all values in the dataset.
It indicates the overall magnitude of the data. The S for age is
76, for gender is 29, for OVAS is 95, for OJOA is 99 and for
OMMC is 95. These Ss represent the cumulative values for
each respective variable.
Summary of 1-week and 6 months (postoperative) in OLFS results
The summary includes measurements taken at two-t me points: 1 week and 6 months postoperative. The variables of interest are OVAS1, OJOA1, OMMC1, OVAS6, OJOA6 and OMMC6.
| OVAS1 | OJOA1 | OMMC1 | OVAS6 | OJOA6 | OMMC6 | |
|---|---|---|---|---|---|---|
| M | 4.75 | 4.8 | 4.55 | 3.8 | 3.85 | 4.15 |
| SE-M | 0.099 | 0.092 | 0.114 | 0.092 | 0.082 | 0.167 |
| MD | 5 | 5 | 5 | 4 | 4 | 4 |
| ME | 5 | 5 | 5 | 4 | 4 | 4 |
| SD | 0.444 | 0.41 | 0.51 | 0.41 | 0.366 | 0.745 |
| SK | -1.251 | -1.624 | -0.218 | -1.624 | -2.123 | -0.257 |
| SE-SK | 0.512 | 0.512 | 0.512 | 0.512 | 0.512 | 0.512 |
| KT | -0.497 | 0.699 | -2.183 | 0.699 | 2.776 | -1.043 |
| SE-KT | 0.992 | 0.992 | 0.992 | 0.992 | 0.992 | 0.992 |
| R | 1 | 1 | 1 | 1 | 1 | 2 |
| S | 95 | 96 | 91 | 76 | 77 | 83 |
Table 10: Statistical summary for 1 week and18 months (post-operative).
• Mean: The mean represents the average value of the
measurements. At 1 week postoperative, the mean scores
were 4.75 for OVAS1, 4.80 for OJOA1 and 4.55 for OMMC1.
At 6 months postoperative, the mean scores were 3.80 for
OVAS6, 3.85 for OJOA6 and 4.15 for OMMC6.
• Std. error of mean: This value indicates the standard error
associated with the mean estimate. It quantifies the
variability or uncertainty in the mean value. Smaller values
indicate greater precision in the estimation.
• Median: The MD represents the middle value in the data set
when arranged in ascending order. It provides a measure of
central tendency that is less affected by extreme values. In
this case, the MD scores were 5.00 for OVAS1, OJOA1, and
OMMC1 at 1 week postoperative, and 4.00 for OVAS6,
OJOA6, and OMMC6 at 6 months postoperative.
• Mode: The ME represents the value that appears most
frequently in the data set. It provides information about the
most common value or category. In this case, the ME for all
variables at both time points was 5, except for OVAS6 and
OJOA6, where the ME was 4.
• Std. deviation: The SD measures the dispersion or variability
of the data points around the mean. A larger SD indicates
greater variability in the data set. The standard deviations
for the variables ranged from 0.366 to 0.745.
• Skewness: SK measures the asymmetry of the data
distribution. Negative SK indicates a longer tail on the left
side of the distribution. In this case, all variables except
OMMC1 and OMMC6 exhibited negative skewness.
• Std. error of skewness: This value indicates the standard
error associated with the SK estimate. It quantifies the
uncertainty in the SK measurement.
• Kurtosis: KT measures the shape of the distribution and
assesses the presence of heavy tails or outliers. Positive KT
indicates a distribution with heavier tails and a more peaked
shape. In this case, all variables except OJOA1 and OMMC6
showed positive KT.
• Std. error of kurtosis: This value indicates the standard error
associated with the KT estimate. It quantifies the
uncertainty in the KT measurement.
• Range: The R represents the difference between the
maximum and minimum values in the data set. In this case,
the R for all variables was 1, except for OMMC6, which had a
R of 2.
• Sum: The S represents the total of all the measurements for
each variable. It provides information on the overall
magnitude of the scores.
Summary of 12 and 18 months (post-operative) in OLFS results
The statistical summary presented in Table 11 provides an overview of the results for OLFS at 12 and 18 months postoperative. The table includes several statistical measures for three outcome variables: OVAS, OJOA, and OMMC.
| OVAS12 | OJOA12 | OMMC12 | OVAS18 | OJOA18 | OMMC18 | |
|---|---|---|---|---|---|---|
| M | 2.65 | 2.85 | 3.25 | 1.3 | 1.45 | 2.05 |
| SE-M | 0.109 | 0.131 | 0.176 | 0.105 | 0.114 | 0.135 |
| MD | 3 | 3 | 3 | 1 | 1 | 2 |
| ME | 3 | 3 | 4 | 1 | 1 | 2 |
| SD | 0.489 | 0.587 | 0.786 | 0.47 | 0.51 | 0.605 |
| SK | -0.681 | 0.004 | -0.496 | 0.945 | 0.218 | -0.012 |
| SE-SK | 0.512 | 0.512 | 0.512 | 0.512 | 0.512 | 0.512 |
| KT | -1.719 | 0.178 | -1.152 | -1.242 | -2.183 | 0.189 |
| SE-KT | 0.992 | 0.992 | 0.992 | 0.992 | 0.992 | 0.992 |
| R | 1 | 2 | 2 | 1 | 1 | 2 |
| S | 53 | 57 | 65 | 26 | 29 | 41 |
Table 11: Statistical summary for 12 and18 months (post-operative).
• Mean: The mean represents the average value for each
outcome variable at 12 and 18 months postoperative. For
example, the mean OVAS score at 12 months is 2.65, while at
18 months, it is 1.30. Similarly, mean values are provided for
OJOA and OMMC scores at both time points.
• Std. error of mean: This measure indicates the precision of
the mean estimates. It represents the SD of the sample means
and is used to assess the reliability of the mean values.
• Median: The MD represents the middle value in the data set.
It provides insight into the central tendency of the
distribution. In this case, the MD values for all outcome
variables are consistent at 3.00 at 12 months and 1.00 at 18
months, except for OMMC, which has a MD value of 4 at 12
months and 2 at 18 months.
• Mode: The ME represents the most frequently occurring value
in the data set. For example, the ME for OVAS, OJOA, and
OMMC scores is 3 at 12 months, indicating that this score
appears most frequently. At 18 months, the ME for OVAS and
OJOA scores is 1, while for OMMC, it is 2.
• Std. deviation: The SD measures the dispersion or variability
of the data set. It provides information about how spreads out
the scores are from the mean. Higher values indicate greater
variability. For instance, the SD for OVAS at 12 months is
0.489, while at 18 months, it is 0.470.
• Skewness: It measures the asymmetry of the data
distribution. Negative indicates that the distribution is skewed
to the left, while positive SK indicates SK to the right. In this
case, OVAS, OMMC and OJOA scores show negative SK at 12
months, but positive SK at 18 months.
• Std. error of Skewness: Similar to the standard error of the
mean, the standard error of SK estimates the precision of the
SK values. It indicates the variability of SK estimates in the
sample.
• Kurtosis: KT measures the peakedness or flatness of the data
distribution. Negative KT indicates a flatter distribution, while
positive KT indicates a more peaked distribution. In this study,
most outcome variables exhibit negative KT values, indicating
relatively flatter distributions.
• Std. error of Kurtosis: The standard error of KT provides
information about the precision of the KT estimates. It
assesses the variability of the KT values in the sample.
• Range: The R represents the difference between the highest
and lowest values in the data set. It provides a measure of the
spread of the scores. In this case, the R is 1-2 for each
outcome variable, indicating the variability in scores between
the two-time points.
• Sum: The values in the table denote the S of scores obtained
for each respective outcome measure at the specified time
points. For example, the S of scores for OVAS12 is 53, OJOA12
is 57, OMMC12 is 65, OVAS18 is 26, OJOA18 is 29 and
OMMC18 is 41.
Comparing efficacy: Endoscopic vs. open lumbar fusion for lumbar stenosis
The efficacy of Fully Endoscopic Lumbar Decompression (FELD) and Open Lumbar Fusion (OLF) in treating lumbar stenosis can be compared by analyzing the statistical results for Visual Analog Scale (VAS), Japanese Orthopaedic Association (JOA) Score and Modified MacNab Criteria (MMC). These measures provide valuable insights into pain relief, functional outcomes and overall surgical success.
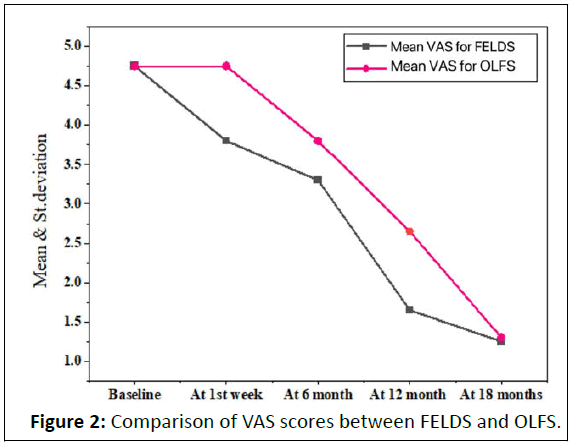
Visual Analog Scale (VAS): The VAS measures pain intensity on a scale from 0 to 10, with higher scores indicating more severe pain. In this comparison, FELDS demonstrated lower mean VAS scores at various time points, suggesting potentially better pain relief compared to OLF. The mean VAS scores for FELDS ranged from 1.25 (at 18 months) to 3.85 (baseline), while for OLF, they ranged from 1.30 (at 18 months) to 4.75 (baseline).
Figure 2 illustrates the comparison of VAS scores between FELDS and OLFS. The results demonstrate that FELDS generally yields lower VAS scores, indicating potentially superior pain relief compared to OLFS. This suggests that patients who undergo FELDS may experience reduced pain levels following the surgery.
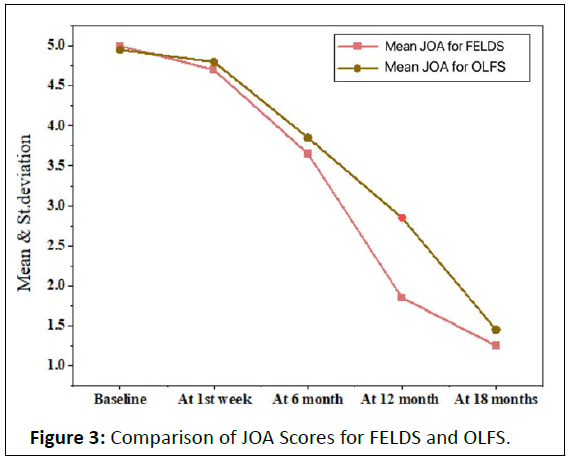
Japanese Orthopaedic Association (JOA) Score: The JOA Score evaluates functional outcomes and neurological improvement. Higher JOA scores indicate better functional outcomes. In this comparison, JOA scores were slightly higher for OLF at most time points, indicating slightly better functional outcomes compared to FELDS. The mean JOA scores for FELDS ranged from 1.25 (at 18 months) to 5.00 (at baseline), while for OLF, they ranged from 1.45 (at 18 months) to 4.95 (at baseline).
Figure 3 displays the comparison of JOA Scores for FELDS and OLFS. Although OLFS shows slightly higher JOA scores, suggesting slightly better functional outcomes, the difference is minimal. Both procedures appear to provide satisfactory functional improvements for patients with lumbar stenosis.
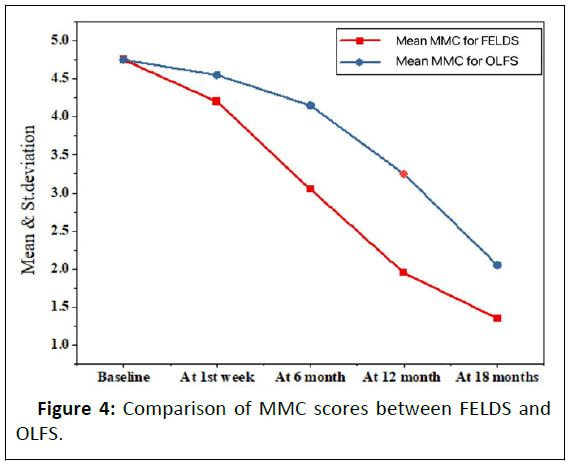
Modified MacNab Criteria (MMC): The MMC evaluates the overall surgical outcome, including pain relief, functional improvement and patient satisfaction. In this comparison, the mean MMC scores were comparable between FELDS and OLFS, indicating similar overall surgical outcomes. The mean MMC scores for FELDS ranged from 1.35 (at 18 months) to 4.75 (at baseline), while for OLFS, they ranged from 2.05 (at 18 months) to 4.75 (at baseline).
Figure 4 depicts the comparison of MMC scores between FELDS and OLFS. The results indicate that MMC scores are comparable between the two procedures, implying similar overall surgical outcomes. This suggests that both FELDS and OLFS result in comparable patient satisfaction and improvement in symptoms after the surgical intervention.
Conclusion
Based on the statistical findings, it can be concluded that fully FELDS and OLFS exhibit distinct strengths in the treatment of lumbar stenosis. FELDS shows promising results in terms of pain relief, as indicated by lower VAS scores. On the other hand, OLFS demonstrates slightly better functional outcomes, reflected in slightly higher JOA scores. However, both procedures yield similar overall surgical outcomes according to MMC scores. These findings provide valuable insights for healthcare professionals in selecting the most suitable surgical approach, considering the individual patient's pain levels, functional status and overall surgical goals.
There are certain limitations to consider in this study. Firstly, the study design introduces inherent biases and potential confounding factors that could impact the results. Secondly, the sample size and patient characteristics may vary across different studies, which can affect the generalizability of the findings. Additionally, the follow-up duration might not be sufficient to capture long-term outcomes and potential complications associated with the procedures. Furthermore, the study may not have accounted for variations in surgeon experience and technique, which could influence the efficacy and outcomes of the surgeries.
To address the limitations and advance the understanding of FELDS and OLFS in treating lumbar stenosis, future research should focus on overcoming the biases through well-designed prospective randomized controlled trials with larger sample sizes. Long-term follow-up studies are necessary to assess the durability of pain relief, functional outcomes, and potential complications. Comparative studies involving standardized surgical techniques and considering surgeon expertise would provide more robust evidence. Additionally, incorporating patient-reported outcomes, such as quality of life measures, and assessing cost-effectiveness would further enhance the understanding of the overall impact of these procedures on patients' well-being.
References
- Andrasinova T, Adamova B, Buskova J, Kerkovsky M, Jarkovsky J, et al. (2018) Is there a correlation between degree of radiologic lumbar spinal stenosis and its clinical manifestation?. Clin Spine Surg 31:E403-408
[Crossref] [Google Scholar] [PubMed]
- Wang Z, Rong Y, Tang P, Ye W, Ji C, et al. (2021) Prevalence and predictive factors of asymptomatic spondylotic cervical spinal stenosis in patients with symptomatic lumbar spinal stenosis. World Neurosurg 151:e1051-1058
[Crossref] [Google Scholar] [PubMed]
- Deer TR, Grider JS, Pope JE, Falowski S, Lamer TJ, et al. (2019) The MIST guidelines: The lumbar spinal stenosis consensus group guidelines for minimally invasive spine treatment. Pain Pract 19:250-274
[Crossref] [Google Scholar] [PubMed]
- Kim HJ, Kim H, Kim YT, Sohn CH, Kim K, et al. (2021) Cerebrospinal fluid dynamics correlate with neurogenic claudication in lumbar spinal stenosis. PLoS One 16:e0250742
[Crossref] [Google Scholar] [PubMed]
- Darlow M, Suwak P, Sarkovich S, Williams J, Redlich N, et al. a pathway for the diagnosis and treatment of lumbar spinal stenosis. Orthop Clin North Am 53:523-534
[Crossref] [Google Scholar] [PubMed]
- Hussein NA, Ahmed KA, Osman NM, Yacoub GE (2022) Role of ultrasonography in screening of spinal dysraphism in infants at risk. J Radiol Nucl Med 53:46
- Ratish S, Gao ZX, Prasad HM, Pei Z, Bijendra D (2018) Percutaneous endoscopic lumbar spine surgery for lumbar disc herniation and lumbar spine stenosis: emphasizing on clinical outcomes of transforaminal technique. Surg Sci 9:63
- Han S, Zeng X, Zhu K, Wu X, Shen Y, et al. (2022) Clinical application of large channel endoscopic systems with full endoscopic visualization technique in lumbar central spinal stenosis: A retrospective cohort study. Pain Ther 11:1309-1326
[Crossref] [Google Scholar] [PubMed]
- Sairyo K, Chikawa T, Nagamachi A (2018) State-of-the-art transforaminal percutaneous endoscopic lumbar surgery under local anesthesia: discectomy, foraminoplasty, and ventral facetectomy. J Orthop Sci 23:229-236
- Paik S, Choi Y, Chung CK, Won YI, Park SB, et al. (2023) Cervical kinematic change after posterior full-endoscopic cervical foraminotomy for disc herniation or foraminal stenosis. PLoS One 18:e0281926
[Crossref] [Google Scholar] [PubMed]
- Wu J, Liu H, Ao S, Zheng W, Li C, et al. (2018) Percutaneous endoscopic lumbar interbody fusion: technical note and preliminary clinical experience with 2-year follow-up. Biomed Res Int 2018:5806037
[Crossref] [Google Scholar] [PubMed]
- Gao G, Cao L, Du X, Xu B, Zhang P, et al. (2022) Comparison of minimally invasive surgery transforaminal lumbar interbody fusion and TLIF for treatment of lumbar spine stenosis. J Healthc Eng 2022:1-2
[Crossref] [Google Scholar] [PubMed]
- Song Q, Zhu B, Zhao W, Liang C, Hai B, et al. (2021) Full-endoscopic lumbar decompression versus open decompression and fusion surgery for the lumbar spinal stenosis: A 3-year follow-up study. J Pain Res 20:1331-1338
[Crossref] [Google Scholar] [PubMed]
- Xue YD, Diao WB, Ma C, Li J (2021) Lumbar degenerative disease treated by percutaneous endoscopic transforaminal lumbar interbody fusion or minimally invasive surgery-transforaminal lumbar interbody fusion: A case-matched comparative study. J Orthop Surg Res 16:1-8
[Crossref] [Google Scholar] [PubMed]
- Gu G, Wang C, Gu X, Zhang H, Zhao Y, et al. (2018) Percutaneous transforaminal endoscopic discectomy for adjacent segment disease after lumbar fusion in elderly patients over 65 years old. World Neurosurg 112:e830-836
[Crossref] [Google Scholar] [PubMed]
- Wu W, Yang S, Diao W, Wang D, Guo Y, et al. (2020) Analysis of clinical efficacy of endo-LIF in the treatment of single-segment lumbar degenerative diseases. J Clin Neurosci 71:51-57
[Crossref] [Google Scholar] [PubMed]
- Jiang Q, Ding Y, Lu Z, Cui H, Zhang J, et al. (2023) Comparative analysis of non-full and full endoscopic spine technique via interlaminar approach for the treatment of degenerative lumbar spinal stenosis: A retrospective, single institute, propensity score-matched study. Global Spine J 13:1509-1521
[Crossref] [Google Scholar] [PubMed]
- Yang Z, Chang J, Sun L, Chen CM, Feng H (2020) Comparing Oblique Lumbar Interbody Fusion with Lateral Screw Fixation and Transforaminal Full-Endoscopic Lumbar Discectomy (OLIF-TELD) and Posterior Lumbar Interbody Fusion (PLIF) for the treatment of adjacent segment disease. Biomed Res Int 2020:4610128.
[Crossref] [Google Scholar] [PubMed]
- Heo DH, Lee DC, Kim HS, Park CK, Chung H (2021) Clinical results and complications of endoscopic lumbar interbody fusion for lumbar degenerative disease: A meta-analysis. World Neurosurg 145:396-404
[Crossref] [Google Scholar] [PubMed]
- Mohamed SH, Essa WM, El-Azeem A, Abdel-Raouf S, Belassy MR (2021) Unilateral fenestration versus open laminectomy in treatment of degenerative stenosis of lumbar spine. Egypt J Hosp Med 82:574-580
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences