Classification of Minimally Invasive Techniques for Transforaminal Lumbar Interbody Fusion
Peyman Pakzaban
DOI10.21767/2471-8173.100025
Peyman Pakzaban*
Houston MicroNeurosurgery, 3801 Vista Rd, Suite 440, Pasadena, TX, USA
- *Corresponding Author:
- Peyman Pakzaban
Houston MicroNeurosurgery, 3801 Vista Rd
Suite 440, Pasadena, TX, USA
E-mail: Pakzaban@live.com
Received date: January 30, 2017; Accepted date: April 28, 2017; Published date: May 02, 2017
Citation: Pakzaban P. Classification of Minimally Invasive Techniques for Transforaminal Lumbar Interbody Fusion. Spine Res. 2017, 3:1. doi:10.21767/2471-8173.100025
Abstract
Several techniques have been described for minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF), offering varying degrees of direct visualization versus reliance on fluoroscopy. In addition, the techniques differ with respect to the extent of neural decompression, choice of fusion substrates, and methods for pedicle screw insertion. Here we classify and contrast these techniques and highlight the features of a recently-described technique known as modified miniopen TLIF (MOTLIF).
Keywords
Fluoroscopy; Tubular retractor; Boney anatomy; Morphogenic protein
Literature Review and Commentary
Minimally-invasive techniques for transforaminal lumbar interbody fusion have been shown to reduce intra-operative blood loss, muscle injury, post-operative pain and length-ofstay and expedite recovery compared to the open technique [1-11]. The main drawback has been increased intra-operative radiation exposure due to reliance on bi-planar fluoroscopy that is required to compensate for diminished surgical exposure and visualization [12-18]. There are several surgical techniques for MIS-TLIF that provide a spectrum of exposures, ranging from minimal to moderate [3-11,19-25]. These are classified as percutaneous techniques, variously described at p-TLIF or MITLIF [3-11], and mini-open techniques, known as o-TLIF [19-25]. Recently, we described a modified mini-open technique, named MOTLIF, which offers an enhanced surgical exposure on par with an open exposure, thereby reducing the need for fluoroscopy [26]. An illustrated technique guide for MOTLIF is available at www.pakzaban.com/MOTLIF_technique_manual [27]. The distinguishing features of p-TLIF, o-TLIF and MOTLIF are outlined in Table 1. Here we compare and contrast these techniques with regard to exposure, decompression, interbody fusion, and pedicle screw placement.
| Technique Abbreviation |
Percutaneous TLIF p-TLIF or MI-TLIF |
Mini-Open TLIF o-TLIF |
Modified Mini-Open TLIF MOTLIF |
|---|---|---|---|
| Incision Placement | Lateral to pedicles | Lateral to pedicles | Overlying pedicles |
| Incision Size | Multiple 1-2 cm incisions | Single 3-4 cm incision | Single 3-4 cm incision |
| or single 3-4 cm incision | |||
| Muscle Handling or Dissection |
Dilation | Dilation | Dissection and detachment from underlying bone |
| Dissection Plane | Inter-muscular | Inter-muscular | Trans-muscular |
| Retractor | Fixed tubular | Fixed or expandable tubular |
Expandable tubular |
| Facetectomy | Piecemeal lateral facetectomy |
Piecemeal subtotal facetectomy |
En-bloc total facetectomy |
| Direct Visualization of Anatomy |
Minimal | Moderate | Enhanced |
| Foraminal Decompression |
Moderate | Enhanced | Enhanced |
| Access for Central Decompression |
Minimal | Moderate | Enhanced |
| Pedicle Screw Insertion |
Over K-wire | With or without K- wire |
Without K-wire |
| Fluoroscopy | Biplanar | Usually Biplanar | Lateral only |
| Fusion substrate | High reliance on BMP | High reliance on BMP | No BMP. Relies on local autograft from en-bloc facetectomy. |
| Additional postero- lateral fusion |
No | No | Optional |
Table 1: Comparison of tTechniques for MIS-TLIF.
Exposure
In p-TLIF and o-TLIF, the incisions are placed lateral to the parasagittal plane of the pedicles and the soft tissues are expanded with the aid of tubular dilators in the cleavage plane between the multifidus and longissimus muscles (inter-muscular approach) to reach the boney anatomy. In MOTLIF, by contrast, a 3 cm incision is placed directly in the parasagittal pedicle plane and a trans-muscular dissection is carried out through the multifidus muscle. Rather than relying on tissue dilators, in MOTLIF the multifidus attachments to bone are cauterized and cut to provide an expansive exposure of the facet joint, pars interarticularis, lateral aspect of lamina and medial aspect of transverse processes. This exposure is then maintained with an expandable tubular retractor that provides a conical field of view that is about 3 cm wide at the skin level and about 6 cm wide at bone level (Figure 1).
In p-TLIF and o-TLIF, the oblique approach trajectory in the intermuscular plane generally requires that the tubular retractor be fixed to the operating table to maintain the approach angle.
In addition, the strong attachments between the multifidus and the underlying bone often lead to muscle creep in the field of view if boney exposures beyond 2 cm to 3 cm are required. In MOTLIF, the vertical trans-muscular trajectory obviates the need for table fixation and allows the expandable retractor to “float” over the boney anatomy as screw drivers and implant inserters are passed through the incision (Figure 1). Furthermore, the expansive boney exposure eliminates muscle creep into the field of view.
Decompression and interbody fusion
In p-TLIF, K-wires are first inserted percutaneously to mark the locations of the pedicles; then a piecemeal lateral facetectomy is carried out to get access to the disc space. This lateral transforaminal approach allows decompression of the neural foramen but not the central canal. The location of the exiting nerve root in such a small transforaminal exposure limits the size of the interbody implant that can be inserted. Most p-TLIF techniques described in the literature rely on bone morphogenic protein (BMP) to achieve interbody fusion [3-11]. Issues regarding the use of BMP have been described extensively [28-33].
o-TLIF compensates for some of the above-mentioned limitations of p-TLIF by providing greater exposure of the boney anatomy which permits a subtotal facetectomy. There is better decompression of the neural foramen and lateral recess and better access for insertion of a properly-sized interbody implant and bone into the disc space. Many surgeons who initially used p-TLIF have developed personal technical variations that fall somewhere in the spectrum between p-TLIF and o-TLIF.
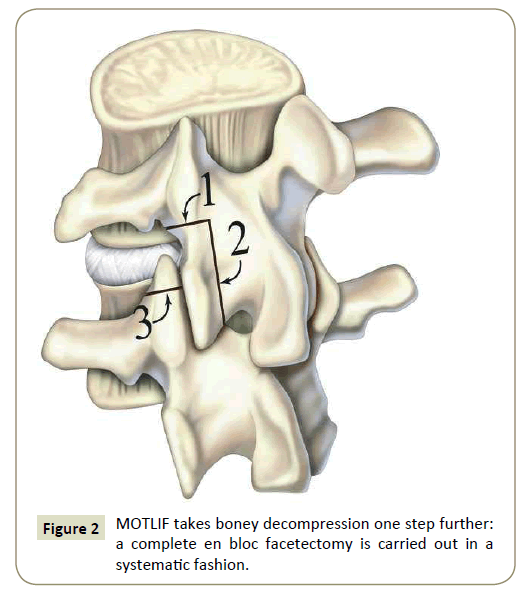
MOTLIF takes boney decompression one step further: a complete en bloc facetectomy is carried out in a systematic fashion (Figure 2). First, a transverse cut is made across the pars interarticularis with a drill or bone scalpel. Second, a sagittal cut is made across the lateral aspect of lamina, allowing removal of the inferior articular process. Third, a transverse cut is made to amputate the tip of the superior articular process. The resulting pedicle-to-pedicle exposure allows complete decompression of the exiting and traversing nerve roots, thorough evacuation of the disc space, and better preparation of endplates for fusion. Furthermore, the bone that has been harvested through enbloc facetectomy is cleaned of its soft tissue attachments and used for interbody fusion. This technique yields abundant high quality bone with high cancellous ratio, especially in patients with hypertrophic facet joints, and obviates the need for BMP. We have reported high fusion rates with MOTLIF, relying only on local facet autograft [26].
Pedicle screw insertion
In p-TLIF, cannulated pedicle screws are inserted over K-wires under bi-planar fluoroscopy. Rod placement may require the use of screw-based guidance devices and a separate skin entry point. In o-TLIF, some authors have described placement of noncannulated screws guided by boney anatomy and fluoroscopy, but most rely on K-wires and bi-planar fluoroscopy as in p-TLIF.
In MOTLIF, the pedicle-to-pedicle exposure and direct visualization of all relevant neural structures allow for free-hand placement of non-cannulated screws, guided only by lateral fluoroscopy, similar to the open technique (Figure 1). This minimizes radiation exposure and permits safe and accurate pedicle screw placement [26]. The rod is placed through the same exposure under direct vision.
Conclusion
Techniques for MIS-TLIF are classified as percutaneous (p-TLIF), mini-open (o-TLIF), and modified mini-open (MOTLIF), respectively offering increasing degrees of direct surgical visualization and decreasing reliance on intraoperative fluoroscopy.
References
- Fan S, Hu Z, Zhao F, Zhao X, Huang Y (2009) Multifidus muscle changes and clinical effects of one-level posterior lumbar interbody fusion: Minimally invasive procedure versus conventional open approach. Eur Spine J 30.
- Kim K, Lee S, Suk K, Bae S (2006) The quantitative analysis of tissue injury markers after mini-open lumbar fusion. Spine 31 :712-716.
- Bagan B, Patel N, Deutsch H (2008) Perioperative complications of minimally invasive surgery (MIS): comparison of MIS and open interbody fusion techniques. Surg Technol Int17:281-286.
- Habib A, Smith ZA, Lawton CD, Fessler RG (2012) Minimally invasive transforaminal lumbar interbody fusion: A perspective on current evidence and clinical knowledge. Minim Invasive Surg657342.
- Holly L,Schwender J, Rouben D, Foley K (2006) Minimally invasive transforaminal lumbar interbody fusion: indications;technique; and complications. Neurosurg Focus20: 6.
- Khoo LT, Palmer S, Laich DT, Fessler RG (2002) Minimally invasive percutaneous posterior lumbar interbody fusion. Neurosurgery51: 166-161.
- OzgurB, Yoo K, Rodriguez G, Taylor W (2005) Minimally-invasive technique for transforaminal lumbar interbody fusion (TLIF). Eur Spine J14 :887-894.
- Park P, Foley K (2008) Minimally invasive transforaminal lumbar interbody fusion with reduction of spondylolisthesis: Technique and outcomes after a minimum of 2 years' follow-up. Neurosurg Focus 25: 16.
- Ringel F, Stoffel M, Stuer C, Meyer B (2006) Minimally invasive transmuscular pedicle screw fixation of the thoracic and lumbar spine. Neurosurgery2:361-366.
- Scheufler KM, Dohmen H, Vougioukas VI (2007) Percutaneous transforaminal lumbar interbody fusion for the treatment of degenerative lumbar instability. Neurosurgery60 :203-212.
- Schwender JD, Holly LT, Rouben DP, Foley KT (2005) Minimally invasive transforaminal lumbar interbody fusion (TLIF): Technical feasibility and initial results. J Spinal Disord Tech1-6.
- Bindal RK, Glaze S, OgnoskiEM, Tunner V, Malone R, et al. (2009) Surgeon and patient radiation exposure in minimally invasive transforaminal lumbar interbody fusion. J Neurosurg Spine11: 375-376.
- Webb J, Gottschalk L, Lee Y, Garfin S, Kim C (2008) Surgeon perceptions of minimally invasive spine surgery. SAS J 2:145.
- Fan G, Fu Q, Gu G (2015)Radiation exposure to surgeon in minimally invasive transforaminal lumbar interbody fusion with novel spinal locators. Jspinal disorders tech28: 173-180.
- Funao H, Ishii K, Momoshima S (2014) Surgeons' exposure to radiation in single- and multi-level minimally invasive transforaminal lumbar interbody fusion; a prospective study. PLoS One 9: 95233.
- Grelat M, Zairi F, Quidet M, Marinho P,Allaoui M, et al. (2015) Assessment of the surgeon radiation exposure during a minimally invasive TLIF: Comparison between fluoroscopy and O-arm system. Neurochirurgie 61:255-259.
- Kim CW, Lee YP, Taylor W, Oygar A, Kim WK (2008) Use of navigation-assisted fluoroscopy to decrease radiation exposure during minimally invasive spine surgery. spine J8:584-590.
- Tumialan LM, Clark JC, Snyder LA, Jasmer G, Marciano FF (2015) Prospective evaluation of a low-dose radiation fluoroscopy protocol for minimally invasive transforaminal lumbar interbody fusion. Neurosurgery.
- Dhall SS, Wang MY, Mummaneni PV (2008) Clinical and radiographic comparison of mini-open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up. J Neurosurg Spine9:560-565.
- Lee DY, Jung TG, Lee SH (2008) Single-level instrumented mini-open transforaminal lumbar interbody fusion in elderly patients. J Neurosurg Spine9:137-144.
- Mummaneni PV, Rodts GE Jr (2005) The mini-open transforaminal lumbar interbody fusion. Neurosurgery256-261.
- Peng CW, Yue WM, Poh SY, Yeo W, Tan SB (2009) Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine34:1385-1389.
- Rodriguez-Vela J, Lobo-Escolar A, Joven-Aliaga E (2009) Perioperative and short-term advantages of mini-open approach for lumbar spinal fusion. Eur spine j18: 1194-1201.
- Scarone P, Lepeintre JF, Bennis S, Aldea S, Dupuy M, et al. (2009) Two-levels mini-open transforaminal lumbar interbody fusion: Technical note. Minim Invasive Neurosurg52:275-280.
- Wu RH, Fraser JF, Hartl R (2010) Minimal access versus open transforaminal lumbar interbody fusion: Meta-analysis of fusion rates. Spine 35: 2273-2281.
- Pakzaban P (2016) Modified mini-open transforaminal lumbar interbody fusion: Description of surgical technique and assessment of free-hand pedicle screw insertion. Spine41: 124-1130.
- Pakzaban P (2010) Mini-open transforaminal lumbar interbody fusion: Surgical technique, pearls, and pitfalls. Aesculap Tech Manual.
- Cahill KS, Chi JH, Day A, Claus EB (2009) Prevalence, complications, and hospital charges associated with use of bone-morphogenetic proteins in spinal fusion procedures 302: 58-66.
- Carter JD, Swearingen AB, Chaput CD, Rahm MD (2009) Clinical and radiographic assessment of transforaminal lumbar interbody fusion using HEALOS collagen-hydroxyapatite sponge with autologous bone marrow aspirate. Spine J9: 434-438.
- Chen NF, Smith ZA, Stiner E, Armin S, Sheikh H (2010) Symptomatic ectopic bone formation after off-label use of recombinant human bone morphogenetic protein-2 in transforaminal lumbar interbody fusion. J Neurosurg Spine12:40-46.
- Ghogawala Z, Benzel EC, Schlenk RP (2010) BMP: A case for evidence and for common sense. Congress Quarterly11:16-17.
- Glassman S, Carreon L, Djurasovic M (2007) Posterolateral lumbar spine fusion with INFUSE bone graft. Spine J7:44-49.
- Kaiser MG, Groff MW, Watters WC (2014) Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 16: Bone graft extenders and substitutes as an adjunct for lumbar fusion. J neurosurg Spine 21:106-132.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences