Ankylosing Spondylitis Versus Internal Disc Disruption: A Case Report Treated Successfully with Intradiscal Platelet-Rich Plasma Injection
Richard G Chang, Nicole R Hurwitz, Julian R Harrison, Jennifer C, and Gregory E Lutz
DOI10.21767/2471-8173.100027
Department of Physiatry, Hospital for Special Surgery, New York, USA
- *Corresponding Author:
- Gregory E Lutz
Department of Physiatry, Hospital for Special Surgery, New York, USA
E-mail: LutzG@HSS.EDU
Received date: February 25, 2017; Accepted date: April 7, 2017; Published date: April 11, 2017
Citation: Chang RG, Hurwitz NR, Harrison JR, et al. Effects of Transcranial Direct Current Stimulation (tDCS) on Chronic Pain in Spinal Cord Injured Patients. Spine Res 2017, 3:3. doi:10.21767/2471-8173.10004
Abstract
We report the case of a 21-year-old female who presented with severe disabling low back pain radiating to both buttocks for 1 year. She was initially diagnosed with ankylosing spondylitis (AS) based on her complaints of persistent low back pain with bilateral sacroiliitis found on magnetic resonance imaging (MRI) of the sacroiliac joints. Despite testing negative for HLA-B27 and lack of other positive imaging to support the diagnosis, she was still treated presumptively as a patient with this disease. These symptoms were debilitating to the point where she withdrew from college, discontinued horseback riding, developed depression, and required antidepressant treatment. She did not improve with oral non-steroid antiinflammatory drugs, neuropathic and opiate pain medications, or a trial of Etanercept (Enbrel). She then presented to our outpatient physiatry office for a second opinion. Her axial low back pain was exacerbated with positions of increased disc load (sitting/lifting/forward bending), and the physical exam was positive for painlimited spine range of motion in flexion greater than extension and dural tension signs. Therefore, a clinical impression was formed that her pain may be more related to an internally disrupted disc (IDD) than AS. This diagnosis was further supported when she failed to obtain any relief with fluoroscopically guided bilateral sacroiliac joint injections. MRI of the lumbar spine was ordered, which revealed a small posterior annular fissure at L5-S1 that was later confirmed as the pain generator with provocative discography. The patient’s pain and function improved transiently with a caudal epidural steroid injection and were significantly alleviated with two serial intradiscal platelet-rich plasma (PRP) injections. The patient returned to college, discontinued anti-depressant and pain medications, and resumed all activities 1 year from the second PRP injection. Additionally, she has had no further treatment of her presumed AS.
Keywords
Ankylosing spondylitis; Annular fissure; Discogenic low back pain; Internal disc disruption; Intradiscal therapies; Platelet-rich plasma; Regenerative medicine; Sacroiliac joint pain; Sacroiliitis
Abbreviations
AS: Ankylosing Spondylitis; IDD: Internal Disc Disruption; IVD: Intervertebral Disc; MRI: Magnetic Resonance Imaging; NSAID: Non-Steroidal Anti- Inflammatory Drug; PRP: Platelet-Rich Plasma; PSIS: Posterior Superior Iliac Spines; SI: Sacroiliac
Introduction
The differential diagnosis of patients who present with primarily low back and bilateral buttock pain without any clear inciting event is wide. In general, common musculoskeletal etiologies that may explain such pain patterns include lumbar discogenic pain from internal disc disruption (IDD), facet arthropathy, myofascial pain, or referred hip pain from greater trochanteric pain syndrome. The sacroiliac (SI) joint is another commonly cited pain generator that may present with similar symptomatology. The prevalence of SI joint pain is reported to be 13% to 15% and as high as 30% in patients who present with both low back and buttock pain [1,2]. Bilateral sacroilitis is even more uncommon and often represents an early, hallmark sign of ankylosing spondylitis (AS), a seronegative spondyloarthropathy. The estimated prevalence of this rheumatologic condition ranges from 0.1 to 1.4% [3]. Differentiating among these numerous conditions may be challenging, but may be further elucidated with an understanding of the known epidemiology and risk factors of these disorders, the gathering of an effective history, the results of a neuromusculoskeletal physical exam, and the judicious use of relevant studies and/or select image-guided injections.
Case Presentation
A 21-year-old female with history of Graves’ disease status following iodine and radiation treatment in 2012 presented with a 1-year history of low back pain radiating to the bilateral buttocks and intermittently to the posterior thighs. Her symptoms started insidiously and were refractory to physical therapy, non-steroidal anti-inflammatory drugs (NSAIDs), Gabapentin, Duloxetine, Enbrel (etanercept), and opiates. The pain was described as constant and severe, and ranged from a scale of 4 to 10 out of 10. It was exacerbated with prolonged standing, walking, or sitting, and was particularly bothersome in the morning. She could not identify any alleviating factors. She denied any lower extremity weakness, bowel/bladder changes, or constitutional symptoms, but endorsed feelings of depression and poor quality of life due to her pain. There was no family history of rheumatologic conditions. In retrospect, she did report being involved in a minor motor vehicle accident 3 months prior to the onset of symptoms.
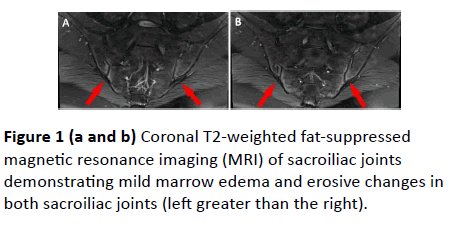
The patient was previously managed with AS by her rheumatologist and was treated for 2 months with Enbrel with no improvement in her symptoms. Her original plain films of the lumbar spine, pelvis, and sacrum did not show any pathognomonic signs of AS, such as vertebral body squaring, syndesmophyte formation and lumbar fusion, or symmetrical sacroiliitis. However, a magnetic resonance imaging (MRI) of the sacrum demonstrated mild bilateral sacroiliitis (left greater than right) with no evidence of ankylosis (Figure 1a and 1b). She did not have any MRI of her lumbar spine before presenting to our clinic. Her blood work was negative for HLAB27, rheumatoid factor, and antinuclear antibody, with normal complement and inflammatory marker levels (C-reactive protein: 34; erythrocyte sedimentation rate: 0.5). She also tested negative for Lyme’s disease, Sjogren’s antibodies, and hepatitis.
On physical exam, the patient had restricted lumbar spine range of motion in all planes, especially with flexion. Hip range of motion was full and pain free. No scoliotic deformities were noted. She had diffuse tenderness to palpation to the lumbar paraspinals at L4-5, L5-S1, and at the posterior superior iliac spines (PSIS) bilaterally. There was no tenderness over the greater trochanteric bursas. No weakness was appreciated on strength testing, with her lower extremity reflexes symmetric without ankle clonus bilaterally. Sensation was intact to light touch in both limbs. Gait was slow, but non-antalgic. Her exam was significant for interspinous tenderness at the lower lumbar levels and mild dural tension in the form of positive bilateral straight leg raise and seated Slump’s testing. These tests reproduced her usual low back and radiating symptoms in an S1 distribution. While provocative tests such as FABER and FADIR testing did not reproduce her pain symptoms. Schober’s testing could not be adequately performed secondary to pain.
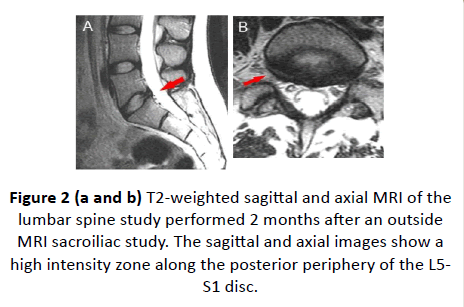
An MRI of the lumbosacral spine was performed 2 months after the MRI of the sacrum. It was significant for an annular fissure at L5-S1 (Figure 2a-2c). It remained unclear whether the pain generator was the presumed sacroiliitis versus an IDD at the L5-S1 segment. Diagnostic fluoroscopically guided bilateral SI injections provided no relief. A fluoroscopic epidural anesthetic and steroid injection was then performed to assess for discogenic low back pain as a result from IDD. We used a caudal approach, because in our experience, this provides the most reliable means of achieving central ventral epidural flow to cover the posterior annulus at the L5-S1 segment. Immediately following the procedure, the patient had anesthetic relief of her low back and radiating buttock pain. One week after the procedure, she reported significant relief for the first time in 1 year. However, this relief was transient and dissipated over the ensuing 3 weeks.
Because the caudal epidural steroid injection was wellreceived, a lumbar discogram was performed to confirm if the symptoms were consistent with IDD at L5-S1. The discogram produced no pain at L4-L5, but did confirm the presence of a symptomatic annular fissure at the L5-S1 level. At the same time as the discogram, we then injected 2 cc of platelet-rich plasma (PRP), which was prepared using the Harvest centrifuge system (Harvest Technologies Corporation, Plymouth, MA), at the L5-S1 level. At 1 month post-PRP injection, the patient reported about 20% improvement in pain symptoms. She also reported a slightly decreased need for Percocet 10/325 mg, which was lowered from 1 tablet 5 times a day to 4 times a day, as well as an increased tolerance for positions that normally would aggravate her symptoms. She was able to tolerate a light physical therapy program for the first time. One month later, she reported decreased depression and pain levels that were 30% of pre-intradiscal PRP pain levels; however, she continued taking pain medications. In collaboration with her rheumatologist, Enbrel was stopped with no change in symptoms.
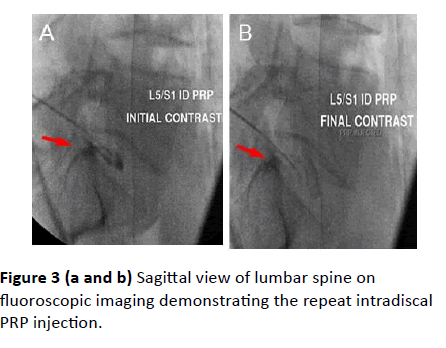
Given her continued, gradual, but positive response to the first intradiscal PRP injection, a repeat intradiscal L5-S1 PRP injection was deemed to be of further therapeutic value (Figure 3a and 3b). The second PRP injection was performed 3 months after the first. She then experienced further improvements in pain and function. Throughout the management course, all interventions were tolerated well without any adverse complications. Two months after the second intradiscal PRP injection, the patient reported intermittent mild pain in the lower back that occasionally radiated to the buttocks. However, these symptoms did not interfere with her daily activities, and she was able to tolerate sitting and standing. She soon progressed to a full physical therapy program, tapered off all pain and anti-depressant medications, and returned to college to pursue her teaching major.
On the 1-year follow-up exam, she had minimal to no tenderness at the L5-S1 interspinous region, no tenderness over the PSIS joints, full, pain-free lumbar spine range of motion, and no neurological deficits. She had returned to full activities and discontinued all opiates.
Discussion
This case highlights the continued importance of a careful, comprehensive medical history, physical exam, and imaging in the diagnostic work-up of patients who present with chronic low back and buttock pain refractory to conservative treatment. As this case illustrates, positive imaging has the potential to mislead physicians to believe the abnormal structure is the primary pain generator. Even though bilateral sacroiliitis is present as a clinical feature in nearly 100% of AS cases, it must be weighed with more commonly encountered musculoskeletal and spine disorders [1]. Although a positive MRI increases the post-test probability of AS to 80% to 95%, this only occurs if patients present with signs and symptoms consistent with inflammatory back pain and positive HLA-B27 serology [4]. The patient presented in the current report did not fulfill all clinical criteria for inflammatory back pain, such as morning stiffness lasting greater than 30 minutes, improvement of back pain with exercise but not rest, or alternating buttock pain [5]. She also had negative serology for HLA-B27. In addition, her radicular pain was not consistent with AS patients. However, if one was to follow the modified New York 1984 criteria for AS, the minimal criteria would have been fulfilled as she did possess restriction of thoracolumbar motion and positive sacroiliitis confirmed on MRI [6,7].
Restriction of motion may be easily explained by her unrelieved pain from IDD. If sacroiliitis was suspected as being responsible for causing the patient’s symptoms, the most facile way to rule in or exclude simple SI joint dysfunction would be a fluoroscopically or computed tomography-guided SI joint injection, which is the gold standard for the diagnosis of SI joint pain [1]. Our patient did not gain any relief from these injections, which suggested that her symptoms were more discogenic in nature.
The incidence of chronic low back pain that is attributable to discogenic causes is reported to be approximately 40% to 45% [8]. Degenerative disc disease begins as early as the second decade of life, and the risk factors include obesity, smoking, and activities involving repetitive lumbar spine flexion and rotation, and or history of trauma [8,9]. Genetic inheritance has also been cited in the development of low back pain [10]. Although the pathophysiology of discogenic pain is not fully understood, a multifactorial model proposes that the combination of decreased disc height, desiccation, reduced proteoglycan content in the nucleus pulposus, and increased mechanical disc pressure loads leads to the disruption of the normal disc architecture, often in the outer third of annulus fibrosis [8,11]. The presence of these defects leads to an inflammatory cascade, followed by a possible compensatory mechanism. The resulting highly innervated disc structure in the setting of a degenerated nucleus pulposus is believed to create this difficult-to-treat pain generator [8]. Vertebral endplate changes are also associated with this cycle (Modic changes on MRI) and appear to be associated with low back pain developing at the level of a disc herniation [12].
Clinically, patients with primarily axial low back pain report symptoms more frequently in the morning hours. The pain is often exacerbated with activities, such as lumbar flexion, prolonged sitting or standing, and Valsalva maneuvers. Lying supine relieves these symptoms [8,13]. The neurologic exam may be unremarkable but may be significant for restricted spine range of motion and dural tension signs. With respect to imaging, the best modality for visualizing disc pathology is MRI. Painful IDD is represented on MRI as a “high intensity zone,” which is an increased T2 signal of the posterior portion of the annulus [14]. However, the “gold standard” diagnostic test for discogenic pain is provocative lumbar discography [8,14]. Although its use has been the subject of debate, it remains to be the only available method of correlating abnormalities seen on MRI with clinically reported pain [8,15]. Initial conservative treatment of chronic discogenic pain consists of a multidisciplinary approach of structured physical therapy, oral pain medications, and patient education. Other complementary treatments, such as chiropractic care, massage, and acupuncture, may be used as adjunct treatment options. Higher-tier treatments include fluoroscopically guided spinal epidural injections, if patients do not improve with the above. Surgical interventions, such as lumbar disc replacement and/or interbody lumbar fusion, are indicated when patients have exhausted all available conservative therapies [16,17].
For patients who suffer from chronic, lumbar discogenic back pain and are not amenable to standard conservative or surgical treatment regimes, intradiscal therapies are a potentially promising option. However, there is an ongoing debate regarding the long-term safety of the procedure, and there is no consensus on what injectate best alleviates discogenic pain without compromising the overall health of the disc [15,18]. The intradiscal injection of stem cells as a possible regenerative therapy has been extensively studied in various animal models of intervertebral disc (IVD) degeneration and is currently being investigated in clinical trials. Despite promising preliminary results, rigorous studies on IVD cells suggest that transplanted cells are unable to survive and adapt in the avascular and hypoxic IVD environment [19]. Thus, the clinical utility of this intradiscal injectate will remain unclear until further research is concluded.
PRP is a biologically active solution that has gained popularity in the treatment of various musculoskeletal injuries and disorders [20,21]. It has been used to successfully heal injured tendons, which are predominantly avascular and are comprised of type I and II collagen. There is evidence to support its efficacy as a treatment in chronic tendinopathies, such as lateral epicondylalgia [22,23] and knee osteoarthritis [24,25]. More recently, PRP has been shown to be effective in the IVD [26,27]. Data in the IVD are promising, but are limited to preliminary studies. Its mechanism of action has not been fully explained, but the various growth factors present in PRP have been suggested to aid in bolstering the healing response to these injuries [17]. In the spine, PRP has historically been used to help augment bony spine fusion [17].
As the largest avascular structure in the human body, IVDs rely primarily on passive diffusion from adjacent endplate vessels for nutrition [28]. Therefore, the IVD has poor inherent healing potential. An analysis of PRP-infused human IVD specimens demonstrated up-regulated cellular proliferation/ differentiation, chondrogenesis, and proteoglycan synthesis [29]. Additionally, intradiscal PRP is associated with greater restoration of disc height, decreased inflammatory cells, and normal cellular architecture in experimentally-injured IVDs in vivo [30]. The injection of fibrin itself may catalyze the sealing of annular fissures [31]. Similarly, in an in vitro study of 5 bovine lumbar IVDs with annular defects, PRP preparations into these areas showed an increase histologically in annular fibrosis matrix and cell production in a course of 4 days [32]. By extension, the intention of injecting PRP in chronic, discogenic disease is to alter the inflammatory environment surrounding the disc and possibly prevent further deterioration and advancement of the degenerative disc cascade [33]. The risks associated with corticosteroid use on the nucleus pulposus and collagenous ring structures are minimized with PRP. Although the risk for further disc degeneration and infection is entirely possible in view of discography, such complications may be avoided when performed in a safe and sterile manner by an experienced physician. In addition, no significant adverse events using this route of delivery have been reported. Another possible beneficial effect of PRP is its impact on circulating systemic growth factors. Although it may be delivered locally to one region of the body, recent studies show that there is an increase in systemic growth factors (albeit temporarily), which theoretically may have an additional anti-inflammatory role [34].
Conclusion
This is the first, known described case of a patient with underlying lumbar discogenic pain with an additional diagnosis of AS, whose pain, quality of life, and function were significantly improved with a novel, regenerative intradiscal therapy consisting of autologous PRP. Clinicians should be both aware of how IDD may masquerade as AS, and how intradiscal PRP may become a promising treatment for patients with IDD. Further long-term randomized controlled studies are needed.
References
- Dreyfuss P, Dreyer SJ, Cole A, Mayo K (2004) Sacroiliac joint pain. J Am Acad Orthop Surg 12: 255-265.
- Schwarzer AC, Aprill CN, Bogduk N (1995) The sacroiliac joint in chronic low back pain. Spine 20: 31-37.
- Braun J, Sieper J (2007) Ankylosing spondylitis. Lancet 369: 1379-1390.
- Carmona R, Harish S, Linda DD, Ioannidis G, Matsos M, et al. (2013) MR imaging of the spine and sacroiliac joints for spondyloarthritis: Influence on clinical diagnostic confidence and patient management. Radiology 269: 208-215.
- Rudwaleit M, Metter A, Listing J, Sieper J, Braun J (2006) Inflammatory back pain in ankylosing spondylitis: A reassessment of the clinical history for application as classification and diagnostic criteria. Arthritis Rheum 54: 569-578.
- Raychaudhuri SP, Deodhar A (2014) The classification and diagnostic criteria of ankylosing spondylitis. J Autoimmun 49: 128-133.
- Rudwaleit M, Khan MA, Sieper J (2005) The challenge of diagnosis and classification in early ankylosing spondylitis: Do we need new criteria? Arthritis Rheum 52: 1000-1008.
- Kallewaard JW, Terheggen MA, Groen GJ (2010) Discogenic low back pain. Pain Pract 10: 560-579.
- Siemionow K, An H, Masuda K, Andersson G, Cs-Szabo G (2011) The effects of age, gender, ethnicity, and spinal level on the rate of intervertebral disc degeneration. A review of 1712 Intervertebral Discs. Spine 36: 1333-1339.
- Battie MC, Videman T (2006) Lumbar disc degeneration: Epidemiology and genetics. J Bone Joint Surg Am 88 Suppl 2: 3-9.
- Urban JPG, Roberts S (2003) Degeneration of the intervertebral disc. Arthritis Res Ther 5: 120-130.
- Albert HB, Manniche C (2007) Modic changes following lumbar disc herniation. Eur Spine J 16: 977-982.
- Allegri M, Montella S, Salici F (2016) Mechanisms of low back pain: A guide for diagnosis and therapy. F1000Research 5:F1000 Faculty Rev-1530.
- Peng B, Hou S, Wu W, Zhang C, Yang Y (2006) The pathogenesis and clinical significance of a high-intensity zone (HIZ) of lumbar intervertebral disc on MR imaging in the patient with discogenic low back pain. Eur Spine J 15: 583-587.
- Carragee EJ, Barcohana B, Alamin T, van den Haak E (2004) Prospective controlled study of the development of lower back pain in previously asymptomatic subjects undergoing experimental discography. Spine 29: 1112-1117.
- Aichmair A, Du JY, Shue J (2014) Microdiscectomy for the treatment of lumbar disc herniation: An evaluation of reoperations and long-term outcomes. Evid Based Spine Care J 5: 77-86.
- Charchian B, Tribuzio B, Zappaterra M, Zall M (2014) Regenerative spinal therapies for low back pain. Curr Phys Med Rehabil Rep 2: 41-47.
- Lu Y, Guzman JZ, Purmessur D (2014) Nonoperative management of discogenic back pain: A systematic review. Spine 39: 1314-1324.
- Sivakamasundari V, Lufkin T (2013) Stemming the degeneration: IVD stem cells and stem cell regenerative therapy for degenerative disc disease. Adv stem cell 724-547.
- Mautner K, Colberg RE, Malanga G (2013) Outcomes after ultrasound-guided platelet-rich plasma injections for chronic tendinopathy: A multicenter, retrospective review. Pm r 5: 169-175.
- Malanga GA and Goldin M (2014) PRP: Review of the current evidence for musculoskeletal conditions. Curr Phys Med Rehabil Rep 2: 1-15.
- Gosens T, Peerbooms JC, van Laar W, den Oudsten BL (2011) Ongoing positive effect of platelet-rich plasma versus corticosteroid injection in lateral epicondylitis: A double-blind randomized controlled trial with 2-year follow-up. Am J Sports Med 39: 1200-1208.
- Thanasas C, Papadimitriou G, Charalambidis C, Paraskevopoulos I, Papanikolaou A (2011) Platelet-rich plasma versus autologous whole blood for the treatment of chronic lateral elbow epicondylitis: A randomized controlled clinical trial. Am J Sports Med 39: 2130-2134.
- Filardo G, Kon E, Buda R, Timoncini A, Di Martino A, et al. (2011) Platelet-rich plasma intra-articular knee injections for the treatment of degenerative cartilage lesions and osteoarthritis. Knee Surg Sports Traumatol Arthrosc 19: 528-535.
- Khoshbin A, Leroux T, Wasserstein D, Marks P, Theodoropoulos J, et al. (2013) The efficacy of platelet-rich plasma in the treatment of symptomatic knee osteoarthritis: A systematic review with quantitative synthesis. Arthroscopy 29: 2037-2048.
- Levi D, Horn S, Tyszko S, Levin J, Hecht-Leavitt C, Levin J, Hecht-Leavitt C, et al. (2016) Intradiscal platelet-rich plasma injection for chronic discogenic low back pain: Preliminary results from a prospective trial. Pain Med 17: 1010-1022.
- Tuakli-Wosornu YA, Terry A, Boachie-Adjei K, Harrison JR, Gribbin CK, et al. (2016) Lumbar Intradiskal Platelet-Rich Plasma (PRP) Injections: A Prospective, Double-Blind, Randomized Controlled Study. Pm r 8: 1-10.
- Urban JP, Smith S, Fairbank JC (2004) Nutrition of the intervertebral disc. Spine 29: 2700-2709.
- Wang SZ, Rui YF, Lu J, Wang C (2014) Cell and molecular biology of intervertebral disc degeneration: current understanding and implications for potential therapeutic strategies. Cell Prolif 47: 381-390.
- Obata S, Akeda K, Imanishi T, Koichi Masuda, Won Bae, et al. (2012) Effect of autologous platelet-rich plasma-releasate on intervertebral disc degeneration in the rabbit anular puncture model: a preclinical study. Arthritis Res Ther 14: 241.
- Allon AA, Aurouer N, Yoo BB, Liebenberg EC, Buser Z, et al. (2010) Structured coculture of stem cells and disc cells prevent disc degeneration in a rat model. Spine J 10(12): 1089-1097.
- Pirvu TN, Schroeder JE, Peroglio M, Verrier S, Kaplan L, et al. (2014) Platelet-rich plasma induces annulus fibrosus cell proliferation and matrix production. Eur Spine J 23: 745-753.
- Wang SZ, Rui YF, Tan Q, Wang C (2013) Enhancing intervertebral disc repair and regeneration through biology: Platelet-rich plasma as an alternative strategy. Arthritis Res Ther 15: 220.
- Wasterlain AS, Braun HJ, Harris AH, Kim HJ, Dragoo JL (2013) The systemic effects of platelet-rich plasma injection. Am J Sports Med 41: 186-193.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences