Impact of Spinal Decompression Therapy on Disability, Pain and Mental Health in Patients with Lumbar Disc Herniation
Yaco Climent Carmona* and Adriano Torres Martin
Individual researchers, Vitalys Center, Spain
- *Corresponding Author:
- Yaco Climent Carmona
Individual researchers,
Vitalys Center,
Spain;
E-mail: sclimentmotril@gmail.com
Received date: January 21, 2023, Manuscript No. IPSR-23-15680; Editor assigned date: January 23, 2023, PreQC No. IPSR-23-15680 (PQ); Reviewed date: February 06, 2023, QC No. IPSR-23-15680; Revised date: February 8, 2023, Manuscript No. IPSR-23-15680 (R); Published date: February 13, 2023, DOI: 10.36648/2471-8173.23.9.1.001
Citation: Carmona YC, Martin AT (2023) Impact of Spinal Decompression Therapy on Disability, Pain and Mental Health in Patients with Lumbar Disc Herniation. Spine Res Vol.9 No.1: 001.
Abstract
The aim of this study was to determine impact of noninvasive spinal decompression therapy on pain, disability and mental health in patients with lumbar disc herniation. A retrospective pilot trial was conducted by an independent clinic in Spain. Questionnaires of 19 patients diagnosed with lumbar disc herniation treated with spinal decompression (BTL Industries Ltd.) treatment protocol were reviewed patient Health Questionnaire-9 (PHQ-9), Visual Analog Scale (VAS) and Oswestry low back pain questionnaire (ODI) as a measure of depression severity, pain perception and disability, respectively. Significant improvement (P<0.05) of all parameters was reported after 6 treatment sessions. PHQ-9 score improved by 66.44%, VAS by 61.15% and ODI by 66.42%. Significant large positive linear relationships (P<0.05) between depression severity and pain and between depression severity and disability were noted. Non-invasive spinal decompression device proved to be an effective tool in treatment of patients with lumbar disc herniation experiencing psychiatric symptoms of various extent in terms of disability, pain and depressive symptoms.
Keywords
Lumbar disc herniation; Mental health; Oswestry disability index; Visual analog scale; Non-invasive spinal decompression
Introduction
Chronic low back pain has become a common problem in industrialized countries. About 61%-83% of adults within younger age groups and 53%-75% in older groups experience low back pain during their lifetime. Recurring symptoms occur in 60%-80% of patients within 1 year and even though most of the patients eventually find relief, some of them may stay with chronic unremitting conditions [1]. Excessive pressure on sciatic nerve, often related to herniated disc, represents about one quarter of all patients suffering from low back pain. Symptomatic lumbar disc herniation is becoming an important socioeconomic burden with lifetime prevalence of about 2%. Adults within the age range 25-55 years are the most prone to herniated disc [2]. Ninety-five percent of all discs herniations happen at level L4-L5 or L5-S1. Lumbar disc herniation is characterized by protrusion of disc material into the spinal canal causing pressure or irritation of the nerve root. Accompanied symptoms include pain of a varying extent and location, sensory abnormalities such as tingling and numbness, decreased muscle strength and movement limitations [3]. Despite these physiological limitations including disability, pain and associated symptoms, there is a significant impact of disc herniation on mental health. Multiple studies have found a relationship between chronic low back pain and depression. Apart from chronic low back pain, symptoms of one or more psychiatric diagnoses were present in 59% of patients. It has also been proven that the degree of depression can have an effect on the success of the treatment [4]. Multiple studies have investigated impact of invasive surgical interventions on PHQ-9 score in patients with lumbar disc herniation, but there is no clinical evidence describing same effect of non-invasive methods. Noninvasive method evaluating impact on PHQ-9 was pelvic floor muscle training in patients with pelvic floor dysfunction. Opinions on associations between baseline mental health and treatment outcomes such as pain and disability differ [5]. Some researchers concluded that there is no significant correlation while others proved an existing significant relationship. The correlation may further be related to different patients' therapy response depending on their severity of depressive symptoms. Such conclusion was suggests that some forms of treatment are more appropriate for patients with severe depression symptoms than others [6].
Currently, the treatment of herniated disc usually consists of pain reducing drugs, a multimodal approach of conventional physiotherapeutic methods and eventually, in case of failure of the first two mentioned, also a surgical intervention. Medication mainly serves to suppress the symptoms and represents the number one choice for most of the patients. For those who want to avoid drugs or find medication insufficient, there is the possibility of conventional physiotherapy [7]. Multimodal approach consisting of manual manipulation, exercise program and application of external energy in form of laser, electrotherapy, magnetic stimulation, diathermy etc. has become popular. Such treatment combining multiple physiotherapy methods proved to be effective in treatment of lumbar disc herniation. Once neither medication nor noninvasive physiotherapy yields desired improvement, surgical intervention is recommended [8]. This proven invasive method has its limitations, such as high costs, long recovery with possible adverse events and complications and its benefit in pain relief compared to conventional physiotherapy is somewhat questionable. Based on findings, surgical intervention is considered to be more effective in short term results of pain management while midterm and long term follow up revealed no significant difference when compared to conservative physiotherapy [9]. Non-surgical spinal decompression therapy represents a non-invasive alternative to decompression surgery. The principle of this new technology is inducing physical changes to the disc by creating segmental distraction during a defined timeframe. Whole process is computer controlled in order to deliver exact decompression force and prevent muscle and ligament overload [10]. Intervertebral space is increased while pressure on the disc is decreased via negative pressure within impaired location. Herniated disc is repositioned and its height is restored [11]. It is believed that the combination of precisely determined force dosage and its delivery to the exact spot is the key in successful treatment. Dosing energy in small increments and treatment couch enabling advanced positioning via multiple movable parts and accessories enables therapists to adapt therapy according to patients' diagnosis. When treating lumbar disc herniation, it is essential to tilt the lumbar area under proper angle in order to target desired location [12]. Most therapists perform the spinal decompression as part of a standard physiotherapy package, thus there is not sufficient clinical evidence evaluating the impact of spinal decompression standalone therapy in patients with lumbar disc herniation. Conducted a retrospective cohort study investigating impact of spinal decompression on pain measured on Verbal Rating Scale (VRS) and disc height obtained by CT scan in patients with discogenic low back pain [13]. After 22 treatment sessions, patients reported significant improvement in pain and CT scans revealed an increase in disc height. Compared effects of spinal decompression with standard traction as an adjunctive therapy to conventional physiotherapy. While there was no significant difference between groups in terms of pain and both treatment programs showed improvement, only spinal decompression standalone therapy proved to increase disc height as shown on MRI. It was concluded by multiple studies that spinal decompression therapy is effective in treatment of patients with lumbar disc herniation [14-17].
Materials and Methods
Current study is a retrospective review of 19 patients treated at free standing clinic in Spain. The Oswestry Disability Index (ODI) questionnaire, Patient Health Questionnaire-9 (PHQ-9) and the Visual Analog Scale (VAS) as a measure of pain intensity were evaluated as a clinic's standard examination package for patients suffering from low back pain [18].
Cooperative male and female adults with lumbar disc herniation were treated with spinal decompression device and subsequently included in the clinical trial. Non cooperative, pregnant and patients with lumbar vertebra fracture, vascular, pulmonary or coronary disease, lumbar canal stenosis, history of lumbar spinal surgery or spinal tumor were not eligible for treatment.
All participants were informed about the course of the treatment prior to signing written informed consent containing agreement with participation and possible results publication [19]. The treatment program was compatible with the 1975 declaration of helsinki ethical guidelines adopted by the general assembly of the world medical association convention on human rights and biomedicine of the council of Europe.
Patients underwent 2 spinal decompression treatments (BTL Industries Ltd.) per week for a 3 weeks period. Therapy was performed in supine, prone or side line position and the patient was fixed to the treatment couch by thoracic or lumbar belt. Angle of the lumbar region was further tilted within the range 0°-25° depending on the exact position of impaired segment. As a next step, a traction test was performed in order to adjust force settings according to patients’ condition and tolerance [20]. Force precision as a key parameter for effectiveness and safety was ensured by 100 grams step increment. It did not exceed 50% of the patient's body weight throughout the treatment. In order to further promote the pain relieving and decompression process, a heating kit, integrated within the treatment couch was applied. After the active part of the therapy, the patient was asked to relax and stabilize in a stable position. Together with the traction test and the subsequent relaxation, the session did not exceed 30 minutes.
Spanish versions of Oswestry low back pain questionnaire and patient health questionnaire-9 were self-filled by participants prior the first and after the last treatment [21]. Patients were further asked to self-assess their pain intensity via Visual Analog Scale (VAS). Oswestry Disability Index (ODI) determines level of disability during everyday activities in patients with low back pain. It is calculated as a sum of score from 10 categories (pain intensity, personal care, lifting, walking, sitting, standing, sleeping, sex life, social life, traveling) multiplied by 2. Patient health questionnaire-9 represents a 9-item PHQ module containing 9 items describing different depressive symptoms and frequency of their manifestation. Number of symptoms prevalent during the last two weeks is essential for assessing diagnosis (major depressive disorder, other depressive disorder, no depressive disorder). Final score within the range 0 to 27 describes the level of depression severity (minimal, mild, moderate, moderately severe, sever). Pain intensity as a selfreported measure of pain was expressed via visual analogue scale. Ten centimeter line represents the pain scale starting with ‘no pain’ on the left and ending with ‘the worst pain’ on the right. Pain level is assessed by measuring the distance in cm between the left end and the patient mark [22].
Data processing for the purpose of statistical analysis was performed in the custom written program (Matlab software processes, Matlab R2010b, mathworks, Inc., Natick, MA, USA). As the data were considered as non-normal by the Shapiro-Wilk test, non-parametric Wilcoxon Paired Test (WPT) was used for evaluation of the significance of the improvement. Pearson coefficient was used for further analysis of correlation between PHQ-9 and VAS/ODI data obtained before the first treatment and association between magnitude of improvements reached during a 3 weeks trial for the same parameters [23].
Despite the standard average across the data (AVG), the difference between the initial and after treatment result was calculated and averaged for ODI, PHQ-9 and VAS (Diff AVG). From this value, the percentage decrease compared to the baseline AVG value was calculated (% decrease).
Results
A total of 19 patients indicated with lumbar disc herniation and treated with non-surgical spinal decompression device were included in the current retrospective clinical study. Six female and 13 male participants with a mean age 50.31 ± 16.03 well tolerated the treatment and reported no adverse events [24].
Visual analog scale
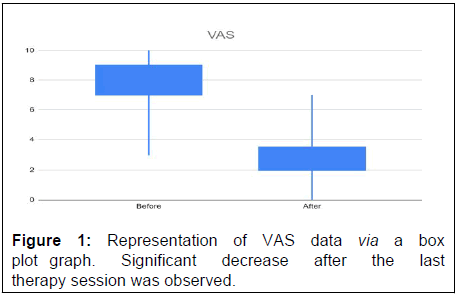
Characteristics of patients’ pain perception assessed via visual analog scale is summarized in Table 1. After 6 treatments, participants reported significant improvement (p<0.05) by 61.15%.
|
|
Visual analog scale | |||
|---|---|---|---|---|
| AVG | Diff AVG | % Decrease | P (0.05) WPT | |
|
Before |
7.32 ± 2.00 |
4.47 ± 1.47 |
61.15% |
0.000187278 |
|
After |
2.84 ± 1.57 |
|||
Table 1: Statistical summary of visual analog scale as a measure of pain perception obtained before and after the spinal decompression treatment program.
VAS data obtained before and after 6 treatment sessions are visualized via box plot in Figure 1.
Oswestry Disability Index (ODI)
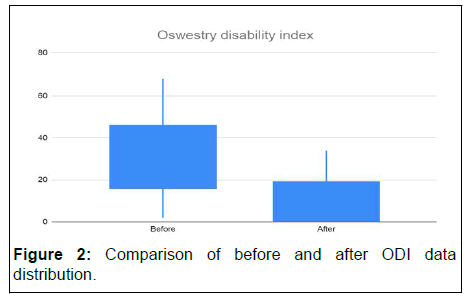
Main statistics of ODI data is summarized in Table 2. Significant improvement (p<0.05) was reached after spinal decompression treatments resulting in decreased disability index by 66.42%.
|
|
Oswestry Disability Index (ODI) |
|||
|---|---|---|---|---|
|
AVG |
Diff AVG |
% Decrease |
P (0.05) WPT |
|
|
Before |
31.62 ± 18.78 |
21.00 ± 13.41 |
0.6642 |
0.000210778 |
|
After |
10.62 ± 11.37 |
|||
Table 2: Characteristics of ODI data obtained at the baseline and after 6 spinal decompression treatment sessions.
Improvement is graphically visualized by box plot graph (Figure 2) comparing data distribution before and after the full treatment program.
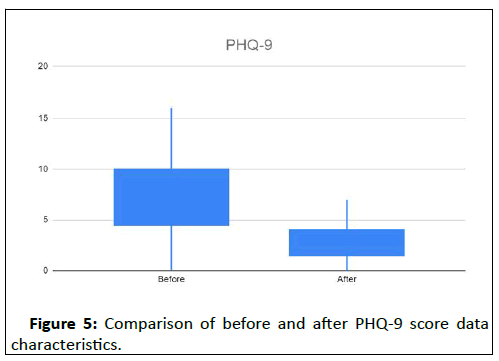
Patient health questionnaire-9
Comparison of PHQ-9 data assessed before and after spinal decompression treatment program revealed significant (p<0.05) improvement by 66.44%Table 3..
|
|
Patient health questionnaire-9 |
|||
|---|---|---|---|---|
|
AVG |
Diff AVG |
% Decrease |
P (0.05) WPT |
|
|
Before |
7.68 ± 4.41 |
5.11 ± 3.94 |
0.6644 |
0.000407575 |
|
After |
2.69 ± 2.20 |
|||
Table 3: Summary of PHQ-9 data statistics obtained at the baseline and after 6 spinal decompression treatment sessions.
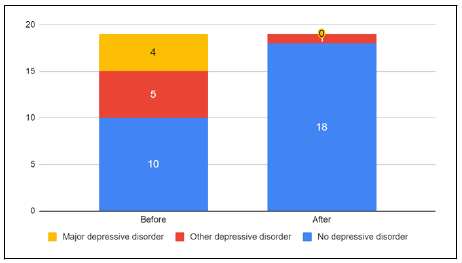
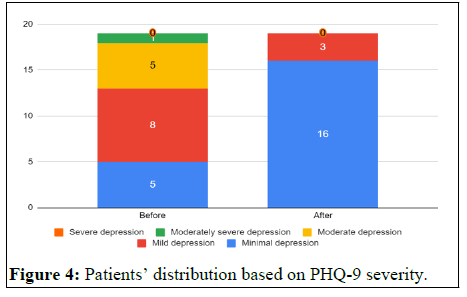
Patients’ diagnosis and severity distributions based on the filled PHQ-9 questionnaires are visualized on Figure 3 and Figure 4, respectively. All patients but 3, reported improvement in depression symptoms. After 6 treatments, there was only a single patient diagnosed with depressive disorder, remaining participants were evaluated as having no depressive disorder. Patients without reported improvement were all diagnosed with no depressive disorder of minimal to mild severity [25-29].
Box plot visualization (Figure 5) of PHQ-9 scores obtained prior the first and after the last treatment confirms significant improvement.
Correlation bteween metnal health and pain/ disability score
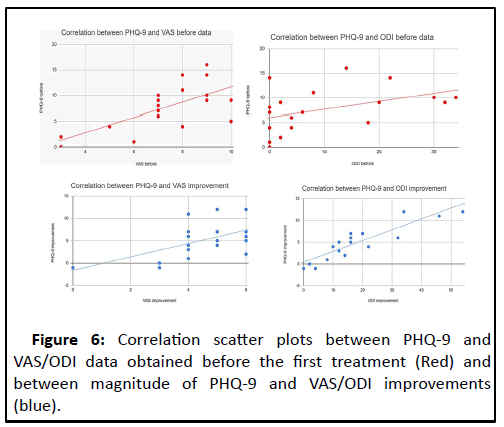
Significant large positive relationship was observed between PHQ-9 and VAS and between PHQ-9 and ODI as data obtained before the first treatment and magnitude improvements were compared (Table 4).
| Before | Improvement | |||
|---|---|---|---|---|
| PHQ-9 and VAS | PHQ-9 and ODI | PHQ-9 and VAS | PHQ-9 and ODI | |
| Pearson coefficient | 0.6665 | 0.8943 | 0.5576 | 0.8888 |
| P value | 0.001833 | 0.0000002424 | 0.01311 | 0.0000003681 |
Table 4: Correlation statistics between PHQ-9 and VAS/ODI. Left columns (before) are comparing data assessed prior to the first appointment while right columns (improvement) are comparing magnitude of improvements reached during the treatment course.
Calculated values of pearson coefficient and corresponding P values are displayed in Table 4. Correlations are visualized via scatter plot in Figure 6.
Discussion
Existing clinical studies have proved the relationship between chronic low back pain and patients’ mental health. Although there is clinical evidence describing impact of surgical interventions on PHQ-9 in patients with lumbar disc herniation, this is the first clinical trial considering the same effect of noninvasive method. Present study confirmed the significant impact of noninvasive spinal decompression treatment on mental health, disability and pain with improvement of 66.44%, 66.42% and 61.15%, respectively in patients with lumbar disc herniation. Post spinal decompression treatment reduction of disability and pain measures is in accordance with existing clinical evidence. Significant improvement in PHQ-9 score was in patients following lumbar surgical decompression and lumbar disectomy, respectivy mean postoperative change ranged from 3.0 ± 5.8 at 12 weeks to 3.6 ± 6.8 at 1 year which is considerably less than the present improvement of 5.11 ± 3.94 of the current trial.
Simple data comparison is not entirely appropriate as multiple factors including the different number of participants, the length of follow up, the difference between invasive and noninvasive approaches and others should be taken into account. Significant large positive linear correlation between PHQ-9 as a measure of depression and Oswestry disability index and between PHQ-9 and visual analog scale as a measure of pain has been found for data obtained at the baseline. Significant strong positive linear relationships were also reported between magnitudes of PHQ-9 and ODI improvements and between magnitudes of PHQ-9 and VAS improvements. Possible explanation for such results might be that disabled patients suffering from pain are more prone to depression and improved physical condition yields reduction of psychiatric symptoms. These findings are aligned with who has found a relationship between depression and physical function measured by PROMIS-PF in patients with lumbar spine stenosis undergoing lumbar decompression surgery. Patients with depressive symptoms were of significantly (P=0.005) worse preoperative disability and pain conditions than patients without depression. Impact of depression on magnitude of disability and pain improvement wasn’t confirmed.
Similarly, evaluated association between symptoms of anxiety and depression and outcomes of pelvic floor muscle training for pelvic floor dysfunction. A strong relationship between the severity of anxiety and depression and the severity of pelvic floor dysfunction was observed. It was also noted that patients who reported the largest improvement were of minimal to mild psychiatric symptoms. This finding contradicts the conclusions of the present study. Possible clarification is based on an assumption supported that as mental health worsens, patients are losing motivation for physical activity. Thus pelvic floor muscle training involving regular exercise might not be the right tool for treatment of depressed patients.
Investigated the relationship between preoperative depression and postoperative outcomes after minimally invasive transforaminal lumbar inter-body fusion. In accordance with the current study, it was noted that higher PHQ-9 scores are associated with higher preoperative disability and pain score. On the other hand, patients with more severe depressive symptoms exhibited less postoperative improvement in both ODI and VAS. Possibly, this finding might be associated with aforementioned loss of motivation in depressed patients. Even though the patient is not actively involved in the surgery itself, his involvement is essential during the recovery period. Lack of motivation and interest can result in insufficient rehabilitation leading to reduced outcomes of surgical intervention. Another explanation might be that the majority of participants in the current trial express only minimal to mild depressive symptoms and therefore any assumption considering severely depressed patients can be somehow biased.
The limitations of this study include absence of a control group for comparing results to untreated or patients treated with other commonly used treatment modality (manual manipulation techniques, stability exercises, medication, etc.), small number of participants and missing follow up period. The number of patients with moderately severe to severe depression symptoms is insufficient as the majority of participants were of minimal to mild depression. Although assessment tools such as visual analog scale, oswestry low back pain questionnaire and patient health questionnaire-9 are considered being rather subjective, these are commonly used among studies with similar focus. Despite aforementioned limitations, this study reported some interesting findings and outlined the direction for further clinical research. A comparison of treatment methods requiring different levels of active involvement of patients with depressive symptoms of various severity might be beneficial.
Conclusion
This retrospective pilot study proved significant impact of noninvasive spinal decompression therapy on disability, pain and as the first also on mental health in patients with lumbar disc herniation. Furthermore, a significant relationship between depressive symptoms and disability/pain measures has been reported. When deciding about the appropriate treatment program for a patient suffering from lumbar disc herniation, it is necessary to take into account not only his physical but also his mental health condition. Methods requiring full patients’ concentration and involvement may not be suitable mainly for patients with more severe symptoms. Noninvasive spinal decompression treatment proved to be an effective tool in treatment of patients with herniated lumbar disc expressing various extent of depressive symptoms.
References
- Cai L, He Q, Lu Y, Hu Y, Chen W, et al. (2019) Comorbidity of pain and depression in a lumbar disc herniation model: Biochemical alterations and the effects of fluoxetine. Front Neurol 10: 1021-1022
[Crossref] [Google Scholar] [PubMed]
- Kao YC, Chen JY, Chen HH, Liao KW, Huang SS (2022) The association between depression and chronic lower back pain from disc degeneration and herniation of the lumbar spine. Int J Psychiatry Med 57: 165-177
[Crossref] [Google Scholar] [PubMed]
- Stubbs B, Koyanagi A, Thompson T, Veronese N, Carvalho AF, et al. (2016) The epidemiology of back pain and its relationship with depression, psychosis, anxiety, sleep disturbances, and stress sensitivity: Data from 43 low and middle income countries. Gen Hosp Psychiatry 43: 63-70
[Crossref] [Google Scholar] [PubMed]
- Amin RM, Andrade NS, Neuman BJ (2017) Lumbar disc herniation. Curr Rev Musculoskelet Med 10: 507-516
[Crossref] [Google Scholar] [PubMed]
- Choi J, Lee S, Hwangbo G (2015) Influences of spinal decompression therapy and general traction therapy on the pain, disability, and straight leg raising of patients with intervertebral disc herniation. J Phys Ther Sci 27: 481-483
[Crossref] [Google Scholar] [PubMed]
- Dydyk AM, Ngnitewe Massa R, Mesfin FB (2022) Disc Herniation. Treasure Island (FL): StatPearls Publishing.
- Dharmajaya R, Sari DK, Ganie RA (2017) A comparison of the quality of sleep between pre and post-surgery cervical herniated nucleus pulposus patients utilizing the anterior discectomy method. Open Access Maced J Med Sci 5: 949-948
[Crossref] [Google Scholar] [PubMed]
- Ma SY, Kim HD (2010) The efficacy of spinal decompression via DRX3000 combined with a spinal mobilization and a lumbar stabilization exercise program for patients with discogenic low back pain. J Phys Ther Sci 22: 345-354
- Gugliotta M, Da Costa BR, Dabis E, Theiler R, Juni P, et al. (2016) Surgical versus conservative treatment for lumbar disc herniation: A prospective cohort study. BMJ Open 6: 012938
[Crossref] [Google Scholar] [PubMed]
- Lynch CP, Cha ED, Jenkins NW, Parrish JM, Geoghegan CE, et al. (2021) Patient health questionnaire-9 is a valid assessment for depression in minimally invasive lumbar discectomy. Neurospine 18: 369
[Crossref] [Google Scholar] [PubMed]
- Khan ZA, Whittal C, Mansol S, Osborne LA, Reed P, et al. (2013) Effect of depression and anxiety on the success of pelvic floor muscle training for pelvic floor dysfunction. J Obstet Gynaecol 33: 710-714
[Crossref] [Google Scholar] [PubMed]
- Parrish JM, Jenkins NW, Cha ED, Lynch CP, Geoghegan CE, e al. (2022) epidemiological relevance of elevated preoperative patient health questionnaire-9 scores on clinical improvement following lumbar decompression. Int J Spine Surg 16: 159-167
- Jacob KC, Patel MR, Cha EDK (2022) Location of Disc Herniation May Affect Outcomes Following Lumbar Decompression. J Orthop Exper Innov The Singh Series: Research in Spine Surgery 1-10
- Danazumi MS (2019) Physiotherapy management of lumbar disc herniation with radiculopathy: A narrative review. Niger J Exp Clin Biosci 7: 92-93
- Soual N (2017) Non-surgical Disc Decompression and Clinical Efficacy. MOJ Orthop Rheumatol 8: 00299
[Crossref]
- Apfel CC, Cakmakkaya OS, Martin W, Richmond C, Macario A, et al. (2010) Restoration of disk height through non-surgical spinal decompression is associated with decreased discogenic low back pain: A retrospective cohort study. BMC Musculoskelet Disord 11: 1-6
[Crossref] [Google Scholar] [PubMed]
- Macario A, Richmond C, Auste M, Pergolizzi JV (2008) Treatment of 94 outpatients with chronic discogenic low back pain with the DRX9000: A retrospective chart review. Pain Practice 8: 11-17
- El-Zayat AR, Gomah W, Aldesouky AH (2019) Spinal decompression therapy as an alternative modality for management of low back pain and radicular pain caused by lumbar disc herniation or protrusion. Egypt Rheumatol 46: 183-188
- Gaowgzeh RAM, Chevidikunnan MF, BinMulayh EA, Khan F (2020) Effect of spinal decompression therapy and core stabilization exercises in management of lumbar disc prolapse: A single blind randomized controlled trial. J Back Musculoskelet Rebill 33: 225-231
[Crossref] [Google Scholar] [PubMed]
- Amjad F, Mohseni-Bandpei MA, Gilani SA, Ahmad A, Hanif A (2022) Effects of nonsurgical decompression therapy in addition to routine physical therapy on pain, range of motion, endurance, functional disability and quality of life versus routine physical therapy alone in patients with lumbar radiculopathy: A randomized controlled trial. BMC Musculoskeletal Disorders 23: 254-255.
[Crossref] [Google Scholar] [PubMed]
- World Medical Assembly (1997) World Medical Association Declaration of Helsinki. JAMA 277: 925-926
- Europe, Council of (1997) Convention for protection of human rights and dignity of the human being with regard to the application of biology and biomedicine: Convention on human rights and biomedicine. Kennedy Institute of Ethics Journal 7:277-290
- Payares K, Lugo LH, Morales V, Londono A (2011) Validation in colombia of the oswestry disability questionnaire in patients with low back pain. Spine 36: 1730-1735
[Crossref] [Google Scholar] [PubMed]
- Wulsin L, Somoza E, Heck J (2002) The feasibility of using the spanish PHQ-9 to screen for depression in primary care in honduras. prim care companion J Clin Psychiatry 4: 190-191
[Crossref] [Google Scholar] [PubMed]
- Delgado DA, Lambert BS, Boutris N, McCulloch PC, Robbins AB, et al. (2018) Validation of digital visual analog scale pain scoring with a traditional paper based visual analog scale in adults. J Am Acad Orthop Surg 2
[Crossref] [Google Scholar] [PubMed]
- Asher R, Mason AE, Weiner J, Fessler RG. (2015) The relationship between preoperative general mental health and postoperative quality of life in minimally invasive lumbar spine surgery. Neurosurgery 76: 672-679
[Crossref] [Google Scholar] [PubMed]
- Merrill RK, Zebala LP, Peters C, Qureshi SA, McAnany SJ (2018) Impact of depression on patient reported outcome measures after lumbar spine decompression. Spine 43: 434-439
[Crossref] [Google Scholar] [PubMed]
- Daley A, Jolly K (2012) Exercise to treat depression. British Med J 344:e3181
- Patel DV, Yoo JS, Khechen B, Haws BE, Block AM (2019) PHQ-9 score predicts postoperative outcomes following minimally invasive transforaminal lumbar interbody fusion. Clin Spine Surg 32: 444-448
[Crossref] [Google Scholar] [PubMed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences