Comparing Outcome Measures in Lumbar Spine Manipulations: Dynamic X-Rays and Oswestry Index
Richard A Roy, Jean P Bouchera and Alain S Comtoisa
DOI10.21767/2471-8173.100012
Richard A Roy1,2, Jean P Bouchera1 and Alain S Comtoisa1
1University of Quebec in Montreal, Department of Kinanthropology, Det Box 8888, Station Centre -Ville, Montreal, Quebec, Canada
2Private Practice, 7655 Newman Boulevard, Suite 205, LaSalle, Québec, Canada
- *Corresponding Author:
- Dr. Richard A Roy
7655 Newman Boulevard, Suuite 205, LaSalle, Quebec, H8N 1X7, Canada.
Tel: 51436417
E-mail: drrichardroy@videotron.ca
Received date: December 01, 2015; Accepted date: January 05, 2016; Published date: January 08, 2016
Abstract
Outcome measurements are used to validate chiropractic adjustments, and they have not always been compared to each other under the same treatment conditions and trials.
Keywords
Manipulation; Diagnostic technique; Oswestry index; Activator
Introduction
Outcome measures have not always been compared to each other under the same treatment conditions and trials [1-3]. This study is needed to evaluate the relative value of comparing two patient evaluation methodologies and determining if one methodology which is less invading to the patient could be used as a reevaluation tool and on-going measurement of patient improvement.
The present evaluation utilized available tools, namely the Oswestry index questionnaire and lateral bending radiographs. Our aim was to determine how the Oswestry index and lateral bending radiographs are affected by treatment, whether either outcome measure could be used as a reevaluation tool, and whether there is a correlation between these two tests. The site of interest for the spinal manipulation was defined as the lumbar spine, defined as the level from T-12 to L-5 according to Maigne [4,5]. Spinal manipulations were done using the Activator Method™ lumbar spine protocol [6,7].
Methods
This study was registered with clinicaltrials.gov, registration number NCT00739570.
Participants
Anthropometric characteristics of the participants are shown in Table 1. The research protocols for the evaluation and adjustment were approved by the Université du Québec à Montréal ethics committee. Written informed consent was obtained from all participants.
| Variables | CTRL | TR |
|---|---|---|
| Weight (kg) | 74.9 ± 16.9 | 80.3 ± 16.5 |
| Height (m) | 1.7 ± 0.1 | 1.7 ± 0.1 |
| BMI | 25.3 ± 3.6 | 28 ± 3.7 |
| Age (Years) | 47.5 ± 16.2 | 45.6 ± 8.9 |
| Values are mean ± SD. CTRL: control group, TR: treatment group | ||
Table 1: Anthropometric measurements of the participants
Control group
A total of ten participants, four females and six males, were recruited in early June 2008 from a chiropractic clinic located at 7655 Newman Boulevard, LaSalle, Quebec. The inclusion criterion was that all participants were receiving maintenance chiropractic care and would not have any treatment during the two-week span of the research project. All participants were examined, x-rayed, and evaluated for all the same outcome measures.
Treatment group
All participants were recruited via an announcement in the newspaper, Le Messager de LaSalle, during the period from July 6th to July 20th 2008. Forty-five subjects called the telephone number at the university and left a message indicating their interest in the project. Eleven participants who met the criteria were selected; the others were thanked for their interest. The eleven participants recruited consisted of four females and seven males. The participants were suffering from a chronic lower back condition at least three months in duration. Chronic back pain can be described as:
“Low back pain that comes and goes over weeks to months. The severity of the pain is always the same. The character of the pain is always the same, cramping pain, sharp or stabbing pain, burning pain and pain that travels to the back”.
All participants were examined, x-rayed, and evaluated for all the same outcome measures. The evaluating chiropractor used static and dynamic palpation, range of motion, physical, neurological, orthopedic, and chiropractic examinations in conjunction with radiographs and the Oswestry index. Those administering the intervention were not blinded to the group assignment.
Materials and Methods
Activities of daily living questionnaire
The modified Oswestry disability index was utilized [8]. It is comprised of ten questions that evaluate the capacity of the patient to function during daily activities and how the patient rates himself on a scale from A to F. The value of A=0, and each subsequent letter has an ascending numerical value, B=1 to F=5. The maximum total score for all ten questions is 50. The total for all the answers is tabulated and multiplied by two to give a percentage of dysfunction due to lumbar pain.
X-ray analysis
X-rays were performed on the participants’ lumbar spine. Anterior-Posterior (AP) lateral bending films in the left and right lateral bending position [9-11] were taken at the end position of the movement, as the patient reached the end position and stopped; the central ray was positioned seven to eight centimeters above the top of the iliac crest. The lateral bending analysis is considered reliable [12]. The lateral film was performed with the central ray at the level of L-5. The radiographs were analyzed by two independent chiropractors. One chiropractor did the pre-treatment analysis, and the other chiropractor did the posttreatment analysis. Both chiropractors were blinded to the group assignment of the participants. The chiropractors would draw lines at the inferior and superior vertebral plates of each vertebra. The lines between the superior aspect of one vertebra and the inferior aspect of the vertebra above it should merge on the side of flexion. If the lines drawn between the superior aspect of one vertebra and the inferior aspect of the vertebra above remained parallel or diverged, this was considered a vertebral dysfunction. The treating chiropractor was allowed to view the radiographs, for treatment, after the initial analyses were completed.
Interventions
A control group was included to isolate the effect of time in the absence of treatment. The participants of the control group received no treatment, only the evaluation of the outcome measures at a two-week interval. In the treatment group, the participants received the previously described chiropractic evaluation and the Activator Method™ evaluation to determine their pelvic deficient (PD) side, which is explained as follows:
“Traditionally, the short leg has been designated the Pelvic Deficient, or PD leg. It is referred to as the reactive leg because of its tendency to appear shorter or longer during different testing procedures. The PD leg is visually observed during the initial leg check following placement of the patient in the prone position on the adjusting Table” [6].
The Activator Method™ basic scan protocol for the lumbar spine was used, and the participants received a chiropractic adjustment.6 The instrument used for the treatment of all patients was an Activator IV Signature (Activator Methods International, Phoenix, Arizona), at the number four setting (176 N),6 and the lumbar area from T-12 to L-5 was treated according to the PD side. The treating clinician held an advanced proficiency rating in the Activator Method™ [13]. The duration of the treatment schedule was two weeks [14].
Experimental Protocol
When the participants arrived for a recording session, they completed the Oswestry index questionnaire. They were asked to remove their clothing except underwear, provided with a cotton gown that had an open slit in the back, and proceeded to the radiology room were the x-rays were taken. This marked the end of the recording session. At the end of the recording session, participants of the control group were instructed to get dressed and made an appointment for the next evaluation in two weeks; the participants of the treatment group then proceeded to make nine appointments to receive chiropractic treatments over the next two weeks [14]. When the patient arrived for a treatment session, they were shown to the treatment room and treated as previously described [6]. After the treatment they would make an appointment for the next day. The participants were treated from Monday, July 28th to Friday, August 1st and then from Monday, August 4th to Thursday, August 7th. Friday, August 8th was the last visit, which consisted of a complete reevaluation where the initial evaluation procedure was repeated. Participant 2109 did not come for the reevaluation. This was the only protocol deviation, and there were no adverse events for all participants throughout the experiment. Our final count for participants was 10 per group. On the last day of recording, all the participants were thanked for their participation and received a $30.00 payment for their travel expenses.
Statistical Analysis
Descriptive statistics (mean ± SD) were computed for all conditions. We also performed a Pearson’s correlation between the different outcome measures [15]. Standardized effect-size calculations were also performed [16,17]. Cohen described an effect size of 0.2 as indicative of a small effect, 0.5 as medium, and 0.8 as a large effect [16]. A general linear model represented by a factorial ANOVA model with repeated measures [15] was used to compare all main effects and interactions (SPSS 15.0, SPSS Inc. Chicago, IL, United States) followed by the student- Newman Keuls test; p < 0.05 was considered as the threshold of statistical significance.
Results
The Activator Method™ analysis revealed the following pelvic deficiency patterns: eightLPD and two RPD in the control group, and four LPD and six RPD in the treatment group. The average number of total segments adjusted per day, from a possible total of 11, decreased from 8.3 ± 1.0 pre-treatment to 3.0 ± 2.6 posttreatment (Table 2), resulting in a standardized effect size of 2.69 for the treatment group.
| level/days | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
| L5 | 9 | 9 | 9 | 10 | 9 | 10 | 10 | 9 | 6 |
| L4 | 7 | 6 | 8 | 10 | 9 | 10 | 7 | 6 | 2 |
| L2 | 9 | 8 | 4 | 2 | 3 | 0 | 1 | 0 | 0 |
| D12 | 8 | 9 | 10 | 10 | 10 | 10 | 9 | 9 | 4 |
| average | 8.3 | 8 | 7.8 | 8 | 7.8 | 7.5 | 6.8 | 6 | 3 |
| SD | 1 | 1.4 | 2.6 | 4 | 3.2 | 5 | 4 | 4.2 | 2.6 |
Average number of segments adjusted per day.
Table 2: Spinal levels and the number of adjustments (maximum = 11) per day from day 1 to day 9, (n = 11 participants).
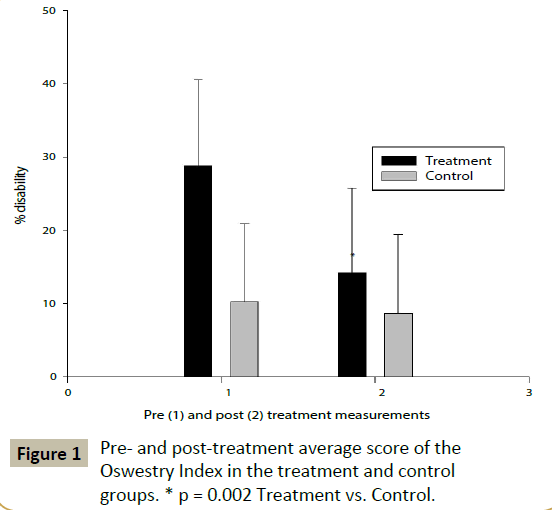
The overall average Oswestry disability index score upon initial and evaluation and reevaluation of the control group were 10.2% ± 10.6% disability and 8.6% ± 10.8% disability, respectively (Figure 1). For the treatment group, the overall average Oswestry disability index score pre- and post-treatment score were 29.8% ± 11.8% disability and 14.20% ± 11.5% disability, respectively (Figure 1). The standardized effect size is 0.15 for the control group and 1.34 for the treatment group.
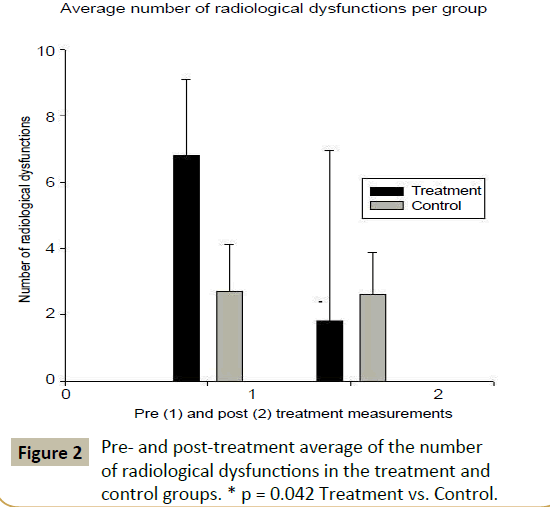
The dynamic x-ray analysis of the control group revealed a total of 27 and 26 dysfunctional segments, respectively, upon radiological initial and reevaluation, from a possible 176 total dysfunctions. The average number of dysfunctional segments in the control group was 2.7 ± 1.4 at initial evaluation and 2.6 ± 1.3 at reevaluation (Figure 2), representing a standardized effect size of 0.07. In the treatment group, the dynamic x-ray analysis revealed a total of 68 dysfunctional segments at the pre-treatment radiological evaluation and a total of 18 at the post-treatment radiological evaluation, from a possible 176 total dysfunctions. The average number of dysfunctional segments decreased from 6.8 ± 2.3 pretreatment to 1.8 ± 5.2 post-treatment (Figure 2), representing a standardized effect size of 1.24. We found a Pearson’s correlation (0.446, p = 0.004) (Table 3) between the number of dysfunctional segments and the Oswestry index. We also found a correlation between the groups (0.324, p = 0.042) and the pre- and posttreatment measurements of dysfunction (-0.500, p = 0.001). The ANOVA analysis (Table 4) resulted in significant findings for the change in the number of radiological dysfunctions for the treatment group (F 1,38 = 4.445, p = 0.042) as well as for the Oswestry index (F1,38 = 10.487, p = 0.002). The Neuman-Keuls test results are illustrated in Figure 3 and reveal that the final Oswestry index measurements between the different groups are similar.
| Dysfunction | Oswestry | |
| Dysfunction | 1 | 0.446 (**) |
| Oswestry | 1 |
Table 3: Pearson’s Correlation between X-ray dysfunction and Oswestry index initial and reevaluation measurements.
Discussion
Patient 2108 from the treatment group had no change in his Oswestry score (30 pre- and post-treatment), but he had only 1 dysfunctional segment remaining at the end of treatment from the initial 9 dysfunctions. The participant mentioned that he felt improvement in his back and had pain in the morning for about 30 minutes upon awakening that then subsided. He wondered if his pain could be related to an inflamed colon, which he had not mentioned initially when asked about additional diseases. The participant said he had been constipated for the last week of treatment. This incident highlights the importance of reevaluation; other diseases may produce pain and mask physical changes related to treatment. Reevaluation is an opportunity to observe and detect other possible painful factors that can affect the patient.
In this experiment the control group demonstrates no real effect and the treatment group demonstrates a very large standardized effect size well above 0.8, the threshold for a large effect [16]. The treatment group revealed the following effect sizes: 1.24 using dynamic x-ray measurements, 1.34 using the Oswestry index, and 2.69 using the number of manipulated segments from the first treatment to the last in the series.
The correlation between the Oswestry index and the functional radiological evaluation (Tables 3 and 4) indicates that this approach could be used as a reevaluation tool. Thus, if the Oswestry index is used as an outcome measure at the beginning of care, re-evaluating the patient with follow-up x-rays is not necessary. This would reduce the expense to the patient or thirdparty payer in addition to reducing radiation to the patient.
| SS | DF | Ss | F | p | ||
|---|---|---|---|---|---|---|
| Dysfunction | Between Groups | 27.225 | 1 | 27.225 | 4.445 | 0.042 |
| Oswestry | Between Groups | 1587.6 | 1 | 1587.6 | 10.487 | 0.002 |
| SS: Sum of Squares, DF: Degree of Freedom, MS: Means of Squares, F: F-value, p: probability of significance. | ||||||
Table 4: ANOVA between Outcome measures and groups.
The strength of our ANOVA (Table 4) for the Oswestry index at p = 0.002 in combination with an effect size of 1.34 indicates that this tool can be used clinically as an assessment tool and as a reassessment tool if included in the initial evaluation. The radiological dysfunction ANOVA is not as strong but still significant (p = 0.042); in combination with its effect size (1.24), this finding indicates that radiological evaluation could also be used as a reassessment tool.
The improvement demonstrated by these results is similar to those obtained by Quon et al. upon treating a patient with side posture manipulation [18]. They report that “the patient improved considerably during only two weeks of treatment,” and “it is emphasized that manipulation has been shown to be an effective treatment for some patients with lumbar disc herniation” [18]. The correlation between different chiropractic techniques’ style of manipulation has often been disputed; however, recently many researchers have demonstrated that different technical approaches produce similar results, in agreement with earlier researchers [3,18-25]. Finally, we can see that without treatment, neither the Oswestry index nor motion x-ray analysis change spontaneously or with time.
Conclusion
Dynamic radiographs and the Oswestry index appear to be sensitive enough to detect a strong effect size after a 9-treatment course of therapy. In addition, a significant correlation was found between pre- and post-treatment measurements of the Oswestry index and dynamic radiographs which could help validate the necessity of continued care.
Acknowledgements
The authors acknowledge the Fondation Chiropratique du Québec (Subvention à la recherche 2005-2006) for their financial support. No other financial support or consideration was received from any organization or commercial entity. In addition, we also wish to thank the two chiropractors who volunteered for the x-ray analysis during our research project, Dr. Charles Clément and Dr. Annette Bourdon. We wish to thank Activator Methods International for the loan of the adjusting instrument, an Activator IV Signature Series.
References
- Owens EF Jr, Hart JF, Donofrio JJ, Haralambous J, Mierzejewski E (2004) Paraspinal skin temperature patterns: an interexaminer and intraexaminer reliability study. J Manipulative PhysiolTher 27: 155-159.
- DeVocht JW, Pickar JG, Wilder DG (2005) Spinal manipulation alters electromyographic activity of paraspinal muscles: A descriptive study. J Manipulative PhysiolTher28:465-471.
- Roy RA, Boucher JP, Comtois AS (2008) Effects of a manually assisted mechanical force on cutaneous temperature.J Manipulative PhysiolTher 31: 230-236.
- Maigne R (1972)Semiotics of minor troubles. Ann Med Phys15:277-289.
- Maigne R (1980) Low back pain of thoracolumbar origin. Arch Phys Med Rehabil 61: 389-395.
- FuhrAW,Fischer RS (2009) The Activator Method. Mosby Elsevier 141-161.
- Freemd.com [Internet]. Rockledge, FL: DSHI Systems, Inc.; c1989-2008 [updated 2008 Dec 26; cited 2009]. Available from: www.freemd.com/chronic-back-pain/definition.htm
- Fairbank JC, Pynsent PB (2000) The Oswestry Disability Index. Spine 25: 2940-2952.
- Cassidy JD (1976)Roentgenological examination of the functional mechanics of the lumbar spine in lateral flexion. J Can ChiroprAssoc13-16.
- Dimnet J, Fischer LP, Gonon G, Carret JP (1978) Radiographic studies of lateral flexion in the lumbar spine.J Biomech 11: 143-150.
- Weitz EM (1981) The lateral bending sign. Spine 6: 388-397.
- Janik T, Harrison DE, Harrison DD, Holland B, Coleman RR, et al. (2001) Reliability of lateral bending and axial rotation with validity of a new method to determine axial rotation on anteroposterior cervical radiographs. J Manipulative PhysiolTher 24: 445-448.
- Fuhr AW and Pavia GR(2008) Activator Methods Chiropractic Technique. Located at: Department of Records. Activator Methods International, Ltd. Arizona 85014.
- Barbuto LM (1984) Industrial back pain and recovery time. J Can ChiroprAssoc28:205-208.
- Kirk RE (1982) Experimental design: procedures for the behavioral sciences. New York: 2nd ed. Brooks/Cole publishing.
- Cohen J(1969) Statistical power analysis for the behavioral sciences. New York: Academic Press.
- Parker RI, Hagan-Burke S (2007) BehavTher 38: 95-105.
- Quon JA, Cassidy JD, O'Connor SM, Kirkaldy-Willis WH (1989) Lumbar intervertebral disc herniation: treatment by rotational manipulation. J Manipulative PhysiolTher 12: 220-227.
- Herzog W (1991) Biomechanical studies of spinal manipulative therapy. J Can ChiroprAssoc35:156-164.
- Herzog W, Conway PJ, Kawchuk GN, Zhang Y, Hasler EM (1993) Forces exerted during spinal manipulative therapy. Spine 18: 1206-1212.
- Symons BP, Herzog W, Leonard T, Nguyen H (2000) Reflex responses associated with activator treatment. J Manipulative PhysiolTher 23: 155-159.
- Herzog W, Kats M, Symons B (2001) The effective forces transmitted by high-speed low-amplitude thoracic manipulation. Spine 26: 2105-2110.
- Wood TG, Colloca CJ and Matthews R (2001) A pilot randomized clinical trial on the relative effect of instrumental (MFMA) versus manual (HVLA) manipulation in the treatment of cervical spine dysfunction. J Manipulative PhysiolTher24:260-271.
- Shearar KA, Colloca CJ, White HL (2005) A randomized clinical trial of manual versus mechanical force manipulation in the treatment of sacroiliac joint syndrome. J Manipulative PhysiolTher28:493-501.
- Kawchuk GN, Prasad NG, McLeod RC, Liddle T, Li T, et al. (2006) Variability of force magnitude and force duration in manual and instrument-based manipulation techniques. J Manipulative PhysiolTher 29: 611-618.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences