Autologous Platelet Rich Plasma for Neck and Lower Back Pain Secondary to Spinal Disc Herniation: Midterm Results
Julian A Cameron* and Katelyn M Thielen
DOI10.21767/2471-8173.100030
Julian A Cameron* and Katelyn M Thielen
Comprehensive Spine Center, PLLC 7710 NW 71 Court Suite 205 Tamarac, USA
- *Corresponding Author:
- Julian A Cameron
Cameron, Comprehensive Spine Center
PLLC 7710 NW 71 Court Suite
205 Tamarac, USA
Tel: (954) 747-1221
E-mail: info@cspinecenter.com
Received Date: June 23, 2017 Accepted Date: July 04, 2017 Published Date: July 10, 2017
Citation: Cameron JA, Thielen KM (2017) Autologous Platelet Rich Plasma for Neck and Lower Back Pain Secondary to Spinal Disc Herniation: Midterm Results. Spine Res. Vol. 3 No. 2:10 doi: 10.21767/2471-8173.100030
Abstract
Background: Spinal disc herniation (HNP) can be a painful condition caused by a variety of traumatic events and degenerative conditions. It is one of the most common spine conditions in adults, occurring in both cervical and lumbar regions. Although these injuries are often associated with wear and tear (or degeneration), traumatic events such as automobile accidents or lifting injuries have been described as causes.
Methodology: We conducted a prospective, nonrandomized, single-center clinical study to evaluate the safety and midterm effectiveness of autologous platelet rich plasma injections (PRP) to treat neck and Low Back Pain (LBP) caused by spinal disc herniation (HNP). All patients had failed conservative treatment for 3 months to 6 months. The autologous PRP was performed using a table top centrifuge device and a standardized individual PRP preparation protocol method. Patients were followed annually for up to 8 years post-operatively. Pain status was documented using a visual analog scale self-reported measure, as well as the Oswestry disability score.
Results: Eighty-eight consecutive patients with spinal disc herniation (HNP) were enrolled; thirty-eight were treated for cervical disc herniation, thirty-eight for lumbar disc herniation, and twelve were treated for both cervical and lumber disc herniation. The duration of follow-up ranged from 4 months to 8 years (mean of 5 years). 87% of patients reported a successful outcome. Within the cervical group, the preoperative visual analog scale showed 81% improvement (P ≤ 0.01). For the lumbar patients, the preoperative visual analog scale improved by 77% (P ≤ 0.01). No complications were reported.
Conclusion: The results are durable with successful outcomes observed 8 years after procedure.
Keywords
Platelet rich plasma; Spinal injuries; Herniation; Lumbar; Cervical; Platelet Rich Plasma (PRP)
Introduction
The literature is replete with evidence of an evolving view of the disease from a supernatural to a scientific basis [1]. The ancient Greeks and Egyptians began to take a more naturalistic view [2]. In the 20th century, German pathologist Christian Schmorl studied 10,000 spines and described his finding of disc protrusions as herniation. In 1932, Mixter and Barr are credited with the first operation of a ruptured disc diagnosis [3]. Later works, especially by Weber and Hakelius, showed that many patients with (lumbar) disc herniation would improve without surgical intervention [3] another pivotal movement was the 2006 publication of the initial results of Spine Patient Outcomes Research Trial (SPORT) [4].
Herniated spinal disc is arguably the most common spinal disorder requiring surgical intervention [1]. Vulnerability of the lateral annulus in the flexed, compressed motion segment leads to disruption followed by circumferential tracking of nuclear material and results in either contained or uncontained extrusions in the posterior or posterolateral annulus. This highlights the complexity of the herniation process [5].
Conservative care for the treatment of spinal disc herniation has been well described and is often successful. Treatment consists of rest, ice, and activity modification acute phase. This can be followed with bracing, physical therapy, oral non-steroidal antiinflammatory drugs, topical applications, and injections of cortisone [1,3]. When conservative treatments fail, autologous PRP may be considered. The goals of PRP treatment of spinal disc herniation are pain resolution and a return to pre-injury function [6-9].
Platelet-rich plasma is an orthobiologic that has recently gained popularity as an adjuvant treatment for musculoskeletal injuries [10-18]. It is a volume of fractionated plasma from the patient’s own blood that contains platelet concentrate. Autologous PRP injections were reportedly first used in 1987 in an open-heart surgery [19]. It was also used, over 20 years ago, in the dental field for promoting accelerated wound healing in cancer patients following jaw reconstruction. Physicians have used PRP to aid bone healing after spinal injury and soft tissue recovery following plastic surgery. PRP gained broad popularity in early 2009 when it was reported that two of the Pittsburg Steelers received PRP for their ankle injuries before their triumph at the Super Bowl [20,21].
PRP was a major initial step that led researchers to consider bone marrow aspirates and stem cells in the growing field of orthobiologics [10]. The role of PRP in the directed stimulation of musculoskeletal and mesenchymal stem cells is being widely investigated and shows promise as a short-term use agent that may assist in the simultaneous healing of several musculoskeletal tissues with trauma or elective surgery [6,14-16].
Based on the pioneering and long-term clinical experience of the oromaxillary field with PRP, and the thousands of patients being treated so far, the use of PRP is considered to be safe [22,23]. Since PRP is prepared from autologous blood, theoretically there are minimal risks for disease transmissions, immunogenic reactions or cancer [4]. In the musculoskeletal field, although no long-term outcome studies with PRP exist, a large number of patients have been treated worldwide [24-27]. In our review of the literature we did not come across RCT’s that have comprehensively evaluated the safety of PRP treatment [10].
Materials and Methods
Patients
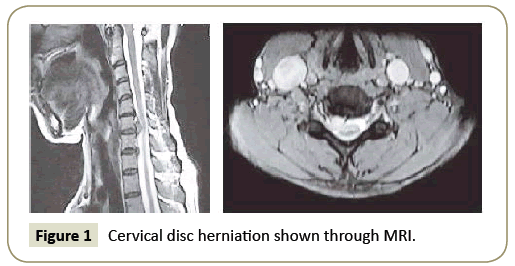
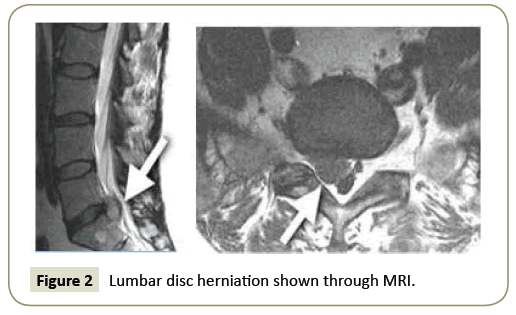
This was a prospective, nonrandomized, single-center clinical study. After receiving institutional review board approval, patients who were 18 years to 65 years of age with neck or back pain with or without radiation and a diagnosis of a confirmed spinal disc herniation with MRI imaging (Figures 1 and 2) were approached for enrollment. For inclusion, patients had to be symptomatic for at least 3 months to 6 months and had to have failed extensive conservative treatments. No operative treatment included activity modification, enrollment in a facility or home-based exercise program, bracing, oral non-steroidal anti-inflammatory medications, and cortisone injection. Candidates with confirmed or suspected pregnancy or with implanted instrumentation adjacent to the target were excluded. A single clinician performed a thorough medical history and clinical evaluation. The clinical follow-up and data collection were performed by an independent medical technician.
Clinical outcomes
Pain status was assessed by using a visual analog scale (VAS). Postoperative clinical assessment was conducted within the first 4 weeks to 6 weeks, at 6 months to 12 months, and up to 8 years postoperatively. The VAS scales were completed annually up to 8 years after the procedure.
The percent improvement of VAS score was calculated. This value represented the difference between the patient’s preoperative and most recent VAS assessments. Failure of the procedure was defined as less than 50% improvement of the VAS score. Tables 1-4 presents the VAS improvement for these patients after the autologous PRP. Pain status was also assessed by using the OSWESTRY disability scoring method for a total of thirty-six patients with a total of forty-two scores. The OSWESTRY scores were completed annually up to 8 years after the procedure.
| VAS Score Improvement (Decrease) | Cervical | Lumbar |
|---|---|---|
| Excellent (≥ 88% decrease) | 28 | 28 |
| Good (75% to 87% decrease) | 4 | 6 |
| Fair (50% to 74% decrease) | 13 | 8 |
| Poor (≤ 50% decrease) | 5 | 8 |
Table 1: Subjective improvement after autologous platelet-rich plasma injection.
| Blood Collection → PRP Prep → Local Injection |
Table 2: The three-step process of PRP treatment.
| OSWESTRY Disability Rating | Cervical | Lumbar |
|---|---|---|
| Excellent (0% to 10% Disability) | 14 | 13 |
| Good (11% to 25% Disability) | 5 | 5 |
| Fair (26% to 35% Disability) | 2 | 1 |
| Poor (≤ 35%) | 1 | 1 |
Table 3: Subjective disability rating after Autologous Platelet -Rich Plasma Injection.
| G-F | Fuction (among many others) |
|---|---|
| (TGF-β) | Stimulates undifferentiated mesenchymal cell (MSC) proliferation |
| (FGF) | Mitogenetic for MSC, chondrocytes, and osteoblasts |
| (PDGF) | Mitogeneteic for MSC and osteoblasts |
| (EFG) Epidermal | Stimulates endothelial chemotaxis or angiogenesis |
| (VEGF) Vascular endo. | Stimulates miotogenesis for endothelial cells |
| (CTGF) Connective tissue | Cartilage regeneration |
| (ILGF 1 and 2) Insulin-like | Chemotactic for fibroblasts and stimulates protein synthesis |
| (PF-4) Platelet factor | Chemo-attractant for fibroblast |
| (IL-8) | Pro-inflammatory mediator |
| (KGF) Keratinocyte | Promote endothelial cell growth, migration, adhesion, and survival |
Table 4: Summary of GF contained in PRP.
The OSWESTRY disability score was calculated. This value represented the patient’s total disability rating following the procedure. Failure of the procedure was defined at an OSWESTRY score over 35%.
Procedure
The senior author performed the procedures in this study. The patient was brought to the operating room and positioned prone. Standard sterile prep and drape were performed prior to initiation of the procedure. We had previously, in the same setting, obtained sterile phlebotomy in order to perform an FDA approved centrifugation at high speed revolutions in order to obtain the autologous platelet rich plasma graft [28]. The patients then had fluoroscopic imaging to confirm the cervical or lumbar levels of the symptomatic area. The patients had the application of topical and local anesthetic injected only in the skin and subcutaneous tissue prior to the grafting. We used needle localization with fluoroscopic imaging to inject the area in a circumferential manner subfascially into the lateral masses, facet joints and lateral gutters and the inter and supraspinatus ligaments, Kambin’s triangle, and spinous processes. The patients were awake throughout and were independently monitored by an anesthesiologist throughout. Aspiration technique was used to avoid any neurologic or vascular compromise or infiltration. Standard wound dressings were applied. In the immediate postop period, the patient was advised to use ice for 48 hours to 72 hours, avoid oral NSAID for 10 days to 14 days, and was advised to begin gentle active ROM exercises.
While avoiding heavy lifting and strenuous physical activity. Each patient was evaluated at 4 weeks postoperatively. At 4 weeks, patients were permitted to increase the intensity of their activities. Return to sports or heavy lifting was allowed once the patient was asymptomatic and had achieved full strength and range of motion; this typically occurred at 6 weeks to 9 weeks postoperatively.
Statistical analysis
Normally distributed data were described using standard parametric statistics (i.e., mean and standard deviation); nonnormally distributed date was characterized using nonparametric descriptors (i.e., median and quartiles). Statistical evaluation of improvement in pain status was performed by calculating 99% confidence intervals and using the Student T test for change between subsequent time points. Use of confidence intervals provides a descriptive analysis of the observed treatment effect, while permitting determination of statistical relevance. In all statistical testing, confidence bounds not including 0 were considered statistically significant. Probability of P ≤ 0.01 for committing type 1 experiment-wise error (rejecting a true null hypothesis) was selected for all statistical testing because of our lack of control group, small sample size, and evaluation of multiple postoperative time points.
Results
Eighty-eight consecutive patients with spinal disc herniation were included in this study. Thirty-eight patients were treated for cervical disc herniation, thirty-eight were treated for lumbar disc herniation, and twelve were treated for both cervical and lumbar disc herniation. The average age of the patients was 50 years. The duration of follow-up evaluation ranged from 4 months to 8 years (mean 5 years).
Within the cervical group, 90% (45/50) of the patient reported a successful outcome. The postoperative VAS improved by 81%. The average OSWESTRY disability rating for the cervical group was 9%. Among the lumbar group, 84% (42/50) reported improvement in symptoms. The postoperative VAS improved by 77%. The average OSWESTRY disability rating for the lumbar group was 8.7%.
Discussion
For the treatment of spinal disc herniation, autologous plateletrich plasma injections are successful in 87% of patients. Symptomatic improvement was observed up to 8 years postoperatively. During this study, no complications were recorded; 13 treatment failures occurred. When compared with other techniques, the results with autologous PRP are equivalent or better.
Regardless of surgical methods and their reported success rate, complications are associated with spinal disc herniation surgery. Post-operative problems may include restricted function, spinal instability, headaches, vasovagal reactions, dural puncture, increased and persistent neck and back pain. Unlike the proposed mechanism of an epidural steroid injection, the effects of PRP occur despite indirect delivery and irrespective of the suspected pain generator. The traditional non-surgical treatment of cortisone injections offers the potential for less morbidity and symptom improvement. However, disadvantages of the cortisone injections include recurrence of the symptoms and increased need for multiple treatments. There has been a reported 16.8% incidence of complication per injection with fluoroscopically guided interlinear cervical epidural injections [29].
Different proposed mechanisms of action have been described to explain the favorable effects of the PRP, such as induced healing by an angiogenic response, inflammatory regulation, cellular stimulation, proliferation and differentiation, as well as tissue regeneration. These factors have been shown to be associated with healing [30-32].
This midterm follow-up of patients with symptomatic spinal disc herniation has shown that autologous PRP can produce successful, durable results. PRP is a technically simple procedure to perform and is associated with a rapid and uncomplicated recovery. It is safe and can effectively eliminate or markedly reduce clinical symptoms.
Limitations
Spinal disc herniation has been described as a self-limited disease, with resolution of symptoms with conservative treatment. This perspective challenges the indication of any proposed surgical or invasive treatment for the condition. Although the results of this research demonstrated the benefits of autologous PRP, there are inherent limitations of the study design. The study lacks a control group, and randomization would improve the strength of the study. Additional outcome measures, such as PROM could complement pain scores to provide more data. Postoperative histologic analysis of treated human tissue would be ideal, but ethical considerations limit study to animal models. An additional limitation is potential examiner bias. Data collection was performed by an independent medical technician, a third-party blinded evaluation could have been performed, but this was not feasible in a clinical setting.
Finally, limitations regarding the lack of description for the PRP variant based on platelet concentration, fibrin concentration, and leukocyte presence and activation status. This omission disadvantages a comprehensive PRP graft assessment. Further analysis of cost effectiveness of PRP is also warranted.
Conclusion
Autologous platelet-rich plasma is a safe and effective procedure for neck and back pain caused by spinal disc herniation. The results are durable with successful outcomes observed 8 years after procedure.
References
- Latka D, Miekisiak G, Jarmuzek P, Lachowski M, Kaczmarczyk J (2016) Treatment of lumbar disc herniation with radiculopathy clinical practice guidelines endorsed by The Polich Society of Spinal Surgery. Neurol Neurochir Pol 50: 101-108.
- Truumeer E (2015) A history of lumbar disc herniationfrom hippocrates to the 1990s. Clin Orthop Rel Res 473: 1885-1895.
- Padura R (1999) The history of the diagnosis and Rx of lumbar sciatic disc herniation. Chir Organi Mov 84: 367-373.
- Deyo R, Tsui-Wu Y (1987) Desciptive epidemiology of LBP and its related medical care in the US. Spine 12: 264-268.
- Van Heeswijk V, Thambyah A, Robertson P, Broom N (2017) Posterolateral disc prolapse in flexion intiated by lateral inner annular failure: An investigation of the herniation pathway. Spine.
- Middleton K, Barro V, Muller B, Terada S, Fu F (2012) Evaluation of the effects of platelet-rich plasma (PRP) therapy involved in the healing of sports-related soft tissue injuries. Iowa Orthop J 32: 150-163.
- Mehta V (2010) Platelet-rich Plasma: A review of the science and possible clinical applications. Orthopedics 33: 111.
- Luga Podesta M, Scott A, Dustin V, Timothy B, Lewis D (2013) Treatment of partial ulnar collateral ligament tears in the elbow with platelet-rich plasma. AM J Sports Med 41: 1689-1694.
- Lacci K, Dardik A (2010) Platelet-rich plasma: Support for its use in wound healing. Yale J Biol Med 83: 1-9.
- Dhillon RS, Schwarz EM, Maloney MD (2012) Platelet-rich plasma therapy- future or trend? Arthritis Res Ther 14: 219.
- Hamilton B, Tol JL, Almusa E (2015) Platelet-rich plasma does not enhance return to play in hamstring injuries: A randomized controlled trial. Br J Sports Med 49: 943-950.
- Reurink G, Goudswaard G, Moen M, Weir A, Verhaar J, et al. (2015) Rationale, secondary outcome scores and 1-year follow-up of a randomised trial of platelet-rich plasma injections in acute hamstring muscle injury: The Dutch hamstring injection therapy study. Br J Sports Med 49: 1206-1212.
- Moraes V, Lenza M, Tamaoki M, Faloppa F, Belloti J, et al. (2014) Platelet-rich therapies for musculoskeletal soft tissue injuries. Cochrane Database Syst Rev 23: 71.
- Kon E, Filardo G, Di Martino A, Marcacci M (2011) Platelet-rich plasma (PRP) to treat sports injuries: Evidence to support its use. Knee Surg Sports Traumatol Arthrosc 19: 516-527.
- Rossi L, Rómoli M, Altieri B, Flor B, Scordo W, et al. (2016) Does platelet-rich plasma decrease time to return to sports in acute muscle tear? A randomized controlled trial. Knee Surg Sports Traumatol Arthrosc
- Hamid MS, Mohamed Ali MR, Yusof A, George J, Lee LP (2014) Plateletrich plasma injections for the treatment of hamstring injuries: A randomized controlled trial. Am J Sports Med 42: 2410-2418.
- Kon E, Filardo G, Delcogliano M, Presti M, Russo A, et al. (2009) Platelet-rich Plasma: New clinical application: A pilot study for treatment of jumper's knee. Injury 40: 598-603.
- Ragab E, Othman A (2012) Platelet-rich plasma for treatment of chronic plantar fasciitis. Arch Orthop Trauma Surg132: 1065-1075.
- Ferrari M, Zia S, Valbonesi M, Henriquet F, Venere G, et al. (1987) A new technique for hemodilution, preparation of autologous platelet-rich plasma and intraoperative blood salvage in cardiac surgery. Int J Artif Org 10: 47-50.
- Praemer A (1999) MS conditions in the US. Rosemont AAOS.
- Banfi G, Corsi M, Volpi P (2006) Could platelet rich plasma have effects on systemic circulation growth factors and cytokine release in orthopaedic application. Br J Sports Med 40: 816.
- Anitua EE, Orive G, Aguirre JJ, Ardanza B, Andía I (2008) 5-year clinical experience with BTI dental implants: Risk factors for implant failure. J Clin Periodental 35: 724-732.
- Anitua EE, Orive G (2010) Short implants in maxillae and mandibles: A retrospective study with 1 to 8 years of follow-up. J Clin Periodental81: 819-826.
- Wang-Saegusa A, Cugat R, Ares O, Seijas R, Cuscó X, et al. (2011) Infiltration of plasma rich in growth factors for osteoarthritis of the knee short-term effects on function and quality of life. Arch Orthop Trauma Surg 131: 311-317.
- Khoshbin A, Leroux T, Wasserstein D, Marks P, Theodoropoulos J, et al. (2013) The efficacy of platelet-rich plasma in the treatment of symptomatic knee osteoarthritis: A systematic review with quantitative synthesis. Arthroscopy 29: 2037–2048.
- Meheux C, McCulloch P, Lintner D, Varner KE, Harris J (2015) Efficacy of Intra-articular platelet-rich plasma injections in knee osteoarthritis: A systematic review. Br J Sports Med 32: 495–505.
- Laudy A, Bakker E, Rekers M, Moen M (2015) Efficacy of platelet-rich plasma injections in osteoarthritis of the knee: A systematic review and meta-analysis. Br J Sports Med 49: 657-672.
- Dhurat R, Sukesh M (2014) Prinicples and methods of preparation of platelet-rich plasma: A review and author's perspecitve. J Cutan Aesthet Surg 7: 189-197.
- Botwin P, Castellanos R, Rao S, Ashraf F, Francisco H, et al. (2003) Complications of fluoroscopically guided interlaminar cervical epidural injections. Arch Phys Med Rehabil 84: 627-633.
- Everts P, Knape J, Weibrich G, Schönberger P, Hoffmann J, et al. (2006) Platelet-rich plasma and platelet gel: A review. J Extra Corpor Technol 38: 174-187.
- Eppley B, Woodell J, Higgins J (2004) Platelete quantification and growth factor analysis from platelet-rich plasma: Implication for wound healing. Plast Reconstr Surg 114: 1502-1508.
- Engebretsen L, Steffen K, Alsousou J, Anitua E, Bachl N, et al. (2010) IOC consensus paper on the use of platelet-rich plasma in sports medicine. Br J Sports Med44: 1072-1081.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences